





|

|
|
|

|
Search
03/19/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
RE: Podiatrists and COVID-19 Pandemic
From: Janet Kail, DPM
Has anyone addressed whether it is advisable to continue seeing non-emergent patients in our offices? So far we are still seeing patients but for the health and safety of all (doctors, staff and patients), what is the opinion of everyone about keeping our private offices open during the COVID-19 crisis)?
Janet Kail, DPM, Fairborn, OH
Other messages in this thread:
02/16/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
RE: EIDL Loans from the SBA
From Corey Fox, DPM
An important reminder to anyone who received an EIDL loan from the SBA: You cannot take distributions from your business or pay bonuses to yourself or your staff for the entire time you have this loan money. It is in the promissory note in very clear terminology. If you need this money, it is a wonderful lifeline to have. If you find you don't really need it, it is better to pay all of it back so you don't get penalized. This does not apply to the HSA grant or the PPP (if you qualify for forgiveness.)
Corey Fox, DPM, Massapequa, NY
01/29/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1B
From: John Chisholm, DPM
I'm sure we all agree on one point: to quote the great Jon Hultman "podiatric physicians are either over-trained or under-licensed". We all agree that "parity" is a necessary but as yet unrealized goal for our specialty. What is challenging for us to agree on is the best strategy for achieving our goal. The California Podiatric Medical Association has been working for years to change our current, restricted license to an unrestricted, plenary license. This strategy would not require a degree change; it would require a different kind of license.
The next hurdle we have to clear is to have podiatric medical students take, and pass, the USMLE or other national licensing exams. I urge all of us to continue to support APMA and state organizations to clear important hurdles so that we can finally have a license that matches our education and training.
John Chisholm, DPM, Chula Vista, CA
01/29/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1A
From: Tilden H Sokoloff, MD, DPM
Leonard Levy DPM, MPH, is spot on. In spite of the “California leadership” working with the California Medical Association and California Orthopedic Association in gaining a plenary license, the issue is bigger than one state.
For our graduates and well trained podiatric physicians to achieve this status, we need a collective stewardship. The APMA has to make this a priority and pull out all the plugs. We have educators, who have the vision, have gone through the process, have ECFMG certification, and have passed the USMLE. Bryan Caldwell MD, DPM is Senior Associate Dean of Academic Affairs at KSUCPM. Daniela Capota MD DPM, practices internal medicine and pediatrics in Florida. I name these people because they are in proximity to schools of podiatric medicine. We have others who are licensed MD DPMs who have finished medical residency programs in the USA with a minimum of additional training in clinical areas.
As Leonard said,” if not now, when?” He knows the “how”. He was Dean, President of many podiatric medical institutions, and osteopathic medical schools. He understands process of accreditation, getting students through the entire process. He is well respected in the medical education community. He started an accredited DPM DO Program at Nova Osteopathic Medical School for podiatric residents. Let’s use our resources well and not reinvent this wheel. Medical education is in disarray, USMLE is redefining how to measure competency and, as of yesterday, the USMLE dropped the clinical skills test permanently. Too much talk and no action = 0. Nurse practitioners have gotten full scope practice licenses in 29 States. We can do this.
Tilden H Sokoloff, MD, DPM, Ketchum, ID
01/28/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
From: Leonard A. Levy, DPM, MPH
Tilden Sokoloff, DPM, MD, says regarding DPMs being able to perform vaccinations, "Time to up the ante and gain a plenary license". There is an old mathematical theory that states, "Things equal to the same thing are equal to each other or 1=1." Podiatric physicians should complete the medical licensing examinations because they are, in fact, physicians (i.e., 1=1).
Our students should complete each of the parts of the medical licensing examinations followed after the first or second year of a podiatric residency by what is now Part 3 of the podiatric medical licensing examinations. This would provide us with the appropriate license and qualify us in our specialty. The time is long overdue.
Leonard A. Levy, DPM, MPH, Ft Lauderdale, FL
01/22/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
RE: Volunteer to be a Vaccinator
From: Steve Abraham, DPM
As part of the NYC Medical Reserve Corp, I gave 220 Moderna vaccine injections over two days, Saturday and Sunday, at the Port Richmond High School on Staten Island. Even though the lines were long, every single person was extremely grateful, thanking us profusely. Our group vaccinated almost 1,500 people in two days.
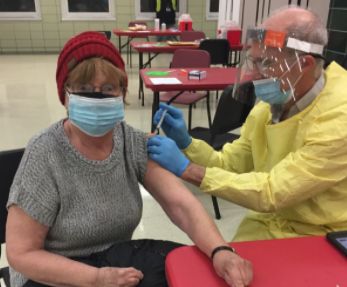 |
Dr. Steve Abraham |
There was a learning curve, as expected, in order to become more efficient as the days progressed. I taught the other vaccinators a more efficient way of injecting, while maintaining aseptic technique. I am volunteering again, as soon as more vaccines become available. We need more vaccinators! Log onto NYC Medical Reserve Corp, register, and you will be rewarded with a rich experience.
Steve E Abraham, DPM, NY, NY
01/21/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1B
From: Elliot Udell, DPM
In this case, both Drs. Levy and Jacobs are correct. Podiatrists are as well trained as any other medical professional in the early management of a severe allergic reaction to any injected medication. As a severe allergy sufferer, I've often asked the professionals who give me my allergy shots how many times they have encountered anaphylaxis. Most said never, but they have guidelines as referenced by Dr. Jacobs hanging in the office, "just in case."
In our office, as with most of my colleagues, we stock epi and injectible antihistamines, and pulmonary support devices and have the protocol hanging in the office. In over thirty years, I have never had to treat a single case of anaphylaxis. On the other hand, I have had to perform CPR three times and was successful two out of the three times and was assured by the ER docs that my only failure had nothing to do with my technique but rather an issue of arriving at the scene way too late.
Elliot Udell, DPM, Hicksville, NY
01/21/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1A
From: Leonard A. Levy, DPM, MPH
I do respect the comments of Allen Jacobs, DPM, but DPMs do need to be careful about what they say. Whether we administer vaccines or any of the many other drugs we may employ (and my understanding is that we are indeed allowed and hopefully capable of safely administering other drugs by mouth and parenterally), we also need to be able to be prepared for adverse reactions that patients may experience. If we are not, then it may be questioned by others as to why we are so permitted to administer such agents.
A large percent of COVID-19 vaccinations are given by pharmacists and many other healthcare workers who are not specialty trained physicians. Furthermore, we are experiencing what is perhaps the most serious public health emergency in the history of the world and almost a quarter of all COVID-19 deaths have occurred in the U.S. The capabilities of the podiatric physician should not be under-estimated.
Leonard A. Levy, DPM, MPH, Ft. Lauderdale, FL
01/20/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1B
From: Allen Jacobs, DPM
Dr. Levy suggests that podiatrists are adequately trained and equipped to administer the COVID-19 vaccination. He further suggests that the reluctance to permit the administration of such vaccinations is political, founded in a lack of understanding of the podiatric medical education.
Dr. Levy posits that a simple injection of epinephrine is all that is required for major adverse reaction to the vaccine; anaphylaxis is believed to occur in 1 per 100,000 doses. However, the occurrence of symptoms such as tachycardia, hypotension, cardiovascular collapse, laryngeal edema, nausea, vomiting requires more than epinephrine. Supportive equipment and care must be readily and immediately available.
I believe that he is wrong. A podiatrist is no more capable of screening for or the handling of emergencies than an orthopedic surgeon, urologist, dermatologist, or any office-based community healthcare provider. Clint Eastwood as Dirty Harry famously said, "a man needs to know his limitations." This is a matter of public safety, not a political issue. I suggest those who are considering administering the vaccination read this.
Allen Jacobs, DPM, St. Louis, MO
01/20/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1A
From: Elliot Udell DPM
Dr. Levy makes a good point that DPMs are well trained to give IM injections of a vaccine and if there is a manpower shortage, we as a profession could solve the problem. Let’s be honest and take this one step further. A monkey could be taught to give an IM injection. The injections that podiatrists give all day long require knowledge and training. Hence, if the powers that be at the various states get their acts together, we could help solve this very serious problem and really make a difference for our society.
Elliot Udell, DPM, Hicksville, NY
01/18/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
From: Leonard A. Levy, DPM, MPH
Kudos to Richard M. Maleski, DPM, RPh for attempting to be a COVID-19 vaccinator. Unfortunately, DPMs are not credentialed to immunize. The U.S. is in a major crisis in its attempt to immunize the nation’s population and yet such barriers still exist. I call such barriers ridiculous although perhaps irresponsible may be a better term. If a DPM decided to use an antibiotic to treat a foot infection, there would not be an outcry. Podiatric physicians have the education, training, and experience to administer intramuscular injections and, in the event of an anaphylactic reaction, can administer epinephrine.
There is no reason to prohibit podiatric physicians, fourth year podiatric medical students, and residents from administering the COVID-19 vaccination except for outdated state regulations often based on ignorance or professional politics. This is especially inappropriate at a time when there is a major shortage of vaccinators when everything possible needs to be done to administer the immunization as quickly as possible to prevent the deaths of thousands of people. If 10,000 DPMs provided about three hours a week to voluntarily administer the immunization over a 90-day period, they would have provided the vaccine to about 2 million people. It also would not hurt for the lay and professional public to know that podiatric medicine has a major role in defeating the pandemic.
Leonard A. Levy, DPM, MPH, Ft. Lauderdale, FL
01/15/2021
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
From: Richard M. Maleski, DPM, RPh
I tried to volunteer to be a vaccinator for COVID-19, but unfortunately in Pennsylvania, DPMs are not credentialed to immunize. There was to be an attempt to get this on an emergency basis, but that never came to fruition. I also still maintain an active pharmacy license, and was going to get certification to immunize. I applied to CVS, since they are running the community vaccination program in my area. However, they rejected my application.
Pharmacy students are allowed to get certification, and I presume that CVS would much rather use students than someone like myself, probably for financial reasons, although I was willing to do it on a voluntary basis. I just found it to be ironic that a DPM with over 30 years experience, having administered about 40,000 complicated injections (nerve blocks, arthrocentesis, etc.) can't get credentialed to immunize, but a pharmacy student can.
Richard M. Maleski, DPM, RPh, Pittsburgh, PA
12/30/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
From: Robert Scott Steinberg, DPM
When we see a patient, we perform an H&P. We then know their health status. But, what do the patients know about our health status? What is their expectations of our health? It should go without saying that they do not want to catch a disease from us. If they are immunocompromised and pregnant, or a child who is immunocompromised, and we pass measles to them, how would we live with ourselves? What about polio, flu, Haemophilus influenzae type b meningitis, pertussis, rubella, etc.?
I hope you have been covering yourself with PPE from head to toe, for the sake of your patients. What extraordinary measures have you been taking to keep your patients safe? Now that you have made your position on vaccines public, what is your increased liability? Have you informed your hospital of your personal decision not to vaccinate, as well as your employees and or partners?
Robert Scott Steinberg, DPM, Schaumburg, IL
12/29/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
From: Mark Spier, DPM
Is this an April Fool's joke that's 9 months late or possibly 3 months early? Dr. Quezada states "Let nature take its course". That's good advice when growing weeds but hardly appropriate coming from a podiatrist ostensibly licensed in the State of Texas. Does D. Quezada let nature take its course with an ascending cellulitis? Nature's course with an acute compartment syndrome? Does nature resolve acute necrotizing fasciitis? If he's suffering from an acute case of vaccine hesitancy related to the new vaccines for COVID-19, one can understand that.
How about vaccinations that have eliminated diseases that were once a scourge such as polio, smallpox, diphtheria, and measles? If nature's way is his philosophy, does he simply lay his hands on all of his patients and pray with them for divine intervention? If yes, what's the code for that service? Asking for an agnostic friend.
Mark Spier, DPM Reisterstown, MD
12/28/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) 1-C
From: Robert G. Smith DPM, MSc., RPh
I fully respect the opinions and belief systems of learned colleagues, and would like to foster an open dialogue. I wish to offer my opinion centered on Covid-19 vaccine hesitancy and wish to provide a mitigating and buffering response that may be used by podiatric physicians who wish to participate with administering the COVID-19 vaccine, and provide data to their patients as a public health initiative.
As I have viewed this vaccine hesitancy through the eyes of practicing two professions as well as an FDA and DEA advisor, the most widely recognized category of unavoidably unsafe products is prescription drugs. Some courts hold that all medications automatically qualify as unavoidably unsafe on the theory that...
Editor's note: Dr. Smith's extended-length letter can be read here.
12/28/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1B
From: Dieter J Fellner, DPM
I have to concur with Dr. Kass. It seems the Governor was, in making this provision, inadvertently provided with the training and qualification requirements of the British chiropodist as applicable in the mid-1960s. Will someone please provide the Governor the training requirements of a 21st Century podiatrist, USA. That should resolve the issue! Whatever next, perhaps the Governor would like to legislate that the podiatrist may treat the ingrowing toenail under supervision of the pedicurist.
Dieter J Fellner, DPM, Yuma, AZ
12/25/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1B
From: Joseph Martin Quezada, DPM
Within days after the application of Pfizer-BioNTech-mRNA, 2.79% were unable to perform normal daily activities, unable to work, or required medical care from a doctor or healthcare professional. I recommend that doctors review the CDC link and make informed decisions. (cdc.gov/vaccines/acip/) In addition, in 2011, the Supreme Court declared that all vaccine designs are "unavoidably unsafe" and "unavoidably defective" due to "unavoidable adverse side-effects" presumptively caused by defective vaccine "design." The Court held that, even where vaccines are free of "manufacturing" and "labeling" defects, they are nevertheless presumed to come with a risk of "unavoidable adverse side effects" caused by defective "design."
The Court ruled that: (1) "design defects" must be the cause of any and all vaccine injuries and deaths; (2) All "design defects" are unavoidable, along with the resulting harm. In plain English, all vaccines are "unavoidably unsafe" precisely because they are "unavoidably defective." The FDA has never even spelled out in regulations the criteria it uses to decide whether a vaccine is safe and effective for its intended use." [Bruesewitz vs. Wyeth LLC, (2011) 562 U.S. 223]. I would never get a vaccine shot nor give one! I trust in nature (God) and let nature take its course!
Joseph Martin Quezada, DPM, Laredo, TX
12/24/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1B
From: Elliot Udell, DPM
The individual states have to decide what doctors should get the COVID-19 vaccine first. A lot will depend upon the supply of the vaccine. It should not strike us as being unusual that an ophthalmologist was "first on line." Eyecare professionals have a strong disadvantage in this pandemic. Their faces are right up against the faces of their patients which renders them very likely to be infected. The same would apply to dentists, ENT doctors, and GI specialists who do upper endoscopies. Even though podiatrists tend to work close to six feet from patients' noses, make no mistake, we are all at risk from the moment we turn the key in our doors and we should not wait a day to be vaccinated when the offer is given to us.
Elliot Udell, DPM, Hicksville, NY
12/24/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC) - PART 1A
From: Wenjay Sung, DPM, Pete Harvey, DPM
I received my vaccine on Friday and actually was given the opportunity to sign up on the first day for vaccination with the “high risk” medical personnel like ICU, ER, etc. I’m not a “staff” podiatrist at my hospital but I do take ER call and I’m frequently consulted for inpatient services. I don’t believe podiatrists were excluded or I was given preference at my hospital because I’m way too young to be senior in anything.
Wenjay Sung, DPM, Arcadia, CA
If you're on active staff of a hospital, they will inform you of your tier turn after injections have been provided to ER workers and other staff who work closely with COVID patients. Be sure that you are on the hospital email list by checking with the medical staff office. Your hospital’s Covid injection supply will also play a role in the timing. Otherwise, I would check closely with your own family physician.
Pete Harvey, DPM, Wichita Falls, TX
12/04/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
RE: Medical Face Masks: An Overview for General Usage and Simple Guidelines
From: Steven Kravitz, DPM
Editor’s Note: This article appeared in the Academy of Professionals in Wound Healing (APWH) Thanksgiving weekend newsletter and reflects current data through October 2020.
Medical facemasks including the N95 are considered the best overall. But access to them can be difficult. Facemasks that contain valves protect from inhalation but not against exhalation and are now becoming banned in some commercial centers because of increased potential transmission. Facemasks with elastic properties that stretch have not been identified with satisfactory filtration for small particles and are not recommended. There has been increased attention recently for...
Editor's Note: Dr. Kravitz's extended length article can be read here.
11/12/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
RE: MIPS and the COVID-19 Exception
From: Gregory Caringi, DPM
With some research, I learned that there is now an "Extreme and Uncontrollable Circumstances Exception" for 2020. Using COVID-19 as the circumstance (prevented collecting data and impacted performance/cost measures), this will allow us to claim an exemption from all 4 categories (Quality, IA, PI, and Cost) for MIPS 2020. This will result in a neutral payment adjustment for 2022. This is no small exception since a neutral adjustment this year requires 45 points (up from 30). Realistically, it will take 85 points to see any positive adjustment.
Gregory Caringi, DPM, Lansdale, PA
11/06/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
Query: FL License Renewal and COVID-19
For the March 22, 2022 podiatric physician license renewal, has the Florida Board of Podiatric Medicine made any allowances for virtual seminar attendance in lieu of live attendance because of the resurgence of COVID-19 across the country and cancellations of live seminars?
Richard Orlandi, DPM, Lake Grove, NY
10/06/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
RE: Minimizing Risk of Medical Malpractice Liability Related to COVID-19 Pandemic
From: Leonard A. Levy, DPM, MPH
The horrors of the COVID-19 pandemic and its implications on medical practice have led attorneys Megan La Suer and Rob Portman to publish an article for Dermatology World (August 2020) on legal issues and malpractice implications that should be considered by physicians in their clinical practice.
These healthcare attorneys recommend that practices should draft and implement policies and procedures addressing extra precautions that need to be taken to prevent the spread of COVID-19 and otherwise mitigate liability risk. Employees should be required to...
Editor's note: Dr. Levy's extended-length post can be read here.
10/01/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
RE: HHS Finally Announces CARES Reporting Requirements
From: Paul Kesselman DPM
Remember that CARES money you signed up for back in the spring? Remember that you attested to requirements you didn't fully know about because the full details actually weren't all available? Remember being told that if you either signed the attestation or did not sign it, either way you attested?
Now the details of what you actually signed up for are finally available. You start making arrangements to prove that attestation is true...this in particular if you received >$10k and most definitely if you received >$75K. Now is the time to check with your accountant and get all your ducks in a row so that you can file the appropriate returns with the government. Click here for the source.
Paul Kesselman, DPM, Oceanside, NY
08/03/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
RE: COVID-19 and Elective Foot Care
From: Joseph Borreggine, DPM
The longer this COVID-19 pandemic goes on, the more likely those who actually need “elective” or “routine” care are truly putting themselves at risk. Patients who routinely sought medical care and went to their yearly wellness checks, dental cleanings, optometry (eye exams) and ophthalmology (cataract), and monthly podiatry care (nail/callus trimming and needed diabetic foot care) are not doing so as they once did.
Most importantly, those requiring elective surgery have also continually dwindled since this all began. These procedures are very important in the realm of preventive medicine. This is quite unfortunate indeed. Because of this mass reduction in those seeking proper healthcare, the majority of...
Editor's note: Dr. Borreggine's extended-length letter can be read here.
06/30/2020
RESPONSES/COMMENTS (CORONAVIRUS PANDEMIC)
From: George F. Jacobson, DPM
I had open heart surgery on June 18 and was home on Monday. Everybody on my floor was required to wear a mask. I posed the same question whether it's slowing down recovery. Getting out of bed and walking was more difficult wearing a mask. Talking was more difficult wearing a mask. I mentioned the same issue to one of the cardiac nurses and was told that an ER nurse was sent home with CO2 difficulties and hasn't returned. I ordered an oximeter.
George F. Jacobson, DPM, Hollywood, FL
|
| |

|
|
|







