|
|
|
|

|
Search
08/08/2024
RESPONSES/COMMENTS (CLINICAL)
RE: Replace Your Neck Stethoscope with a Hand-Held Doppler to Save Limbs
From: Martin M Pressman, DPM
Podiatry standard of care requires us all to palpate pedal pulses. This standard alone is simply not high enough to get the job of limb preservation done. The following list contains some hard won knowledge acquired over the last 47 years of practice; hard won pearls given freely with the hope that some of the 20,000 subscribers might take notice. This note was motivated by a leg-off case where the podiatrist found +2 pulses and 9 days later the patient had an AK amputation for thrombosis. The current standard of care is pulse palpation. If a Doppler were used, perhaps this could have been avoided.
1. Your cardiologist does not palpate your heart; she uses auscultation with a stethoscope to hear cardiovascular flow abnormalities.
2. We need to up our game and use...
Editor's note: Dr. Pressman's extended-length letter can be read here.
Other messages in this thread:
08/14/2024
RESPONSES/COMMENTS (CLINICAL)
From: Bret Ribotsky, DPM
Marty - I join you in taking this first step that I hopefully everyone did 20 years ago. Today (or at least for the last decade since I was a founder of DermFoot), I’ve been recommending a dermatoscope to replace the proverbial stethoscope. I think Bill Scherer said it best, if you haven’t seen a skin cancer this week in your practice, it has seen you.
Bret Ribotsky, DPM, Fort Lauderdale, FL
08/09/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Paul Kesselman, DPM
Kudos to Dr. Pressman for pointing something out which I have been preaching for my over 40+ years as a clinician. I first came aware of non-invasive vascular technology back in the late 1970s and early ‘80s during my undergraduate medical education at rotations at various VA hospitals in the Chicago area. In those days, the machines were big, bulky, and took up an entire room. Their costs and size relegated them mostly to large clinical or research facilities.
With computer technology, eventually the machinery got more sophisticated and totally paper free and can integrate directly into your computer and eventually into your patient's EMR. Most cost 1/3 of what digital x-rays cost, with many fitting into your briefcase. The current machinery can combine pulse volume recording and photoplethysmography, which are far more sophisticated than...
Editor's note: Dr. Kesselman's extended-length letter can be read here
08/09/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1A
From: Jeffrey Kass, DPM
I’d like to thank Dr. Pressman for the free pearl. I sincerely appreciated the pearl and was ecstatic for the first time someone was not trying to extract money from me. I have also come across patients with palpable pulses who have had stenosis or occlusions and the pearl he has shared is of utmost value.
Jeffrey Kass, DPM, Forest Hills, NY
07/30/2024
RESPONSES/COMMENTS (CLINICAL)
From: Donald Blum, DPM
Send the patient to a dermatologist for biopsy, please.
Reviewing this dermatology website, there are about 14 different items that this could be. Without a detailed history, perhaps using dermoscopy, and yes a nail unit biopsy could give you a more definitive diagnosis.
Donald Blum, DPM, Dallas, TX
05/03/2024
RESPONSES/COMMENTS (CLINICAL)
From: Howard Bonenberger, DPM
I appreciated the comments by Jeffrey Trantalis, DPM, however to be clear, I was writing specifically about FHL. This is worth learning about. Addressing it effectively will not only help your patients, it can grow your practice because your orthotic solved a problem that someone else's did not.
Howard Bonenberger, DPM, Nashua, NH
05/01/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1B
RE: Functional Hallux Limitis
From: Howard Dananberg, DPM
Howard Bonenberger mentioned in a post last week that one of my lectures on functional hallux limitus (FHL) inspired him to treat patients with chronic postural complaints. I appreciate his comments and am glad he was able to find these concepts valuable. I have written extensively on FHL over my career, and have come to the realization that this concept remains misunderstood. The reason why it can impact postural form lies in the following principle. Once the hallux makes ground contact during any step, IT DOES NOT MOVE AGAIN UNTIL TOE-OFF. ln any form of hallux limitus (structural or functional), what is restricted is not the hallux, but the remainder of the foot and proximal structures all the way to the neck.
As the body adjusts for these motions, various sites are stressed repeatedly during each step cycle. And since these motions are repeated thousands of cycles per day, the stress becomes a chronic irritant. In particular, loss of MTP joint motion restricts heel lift, shortens stride length, and causes the ensuing swing phase to be altered in such a way as to make toe-off mechanically inefficient. Since the iliopsoas is the primary hip flexor at toe-off, and originates directly from the lumbar spine, it becomes the site of pain. The references for this are below.
Howard Dananberg, DPM
05/01/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1A
RE: Functional Hallux Limitis
From: Jeffrey Trantalis, DPM
Howard Bonenberger, DPM hinted about a very important and prevalent condition that is seen in many, if not all, podiatry offices. This is hallux limitus. In the early 1980s, I had a professional NFL receiver come to me with hallux limitus. It was obvious that conservative treatment was the only option. At that time, orthotics with a hallux extension was the recommended treatment. So I tried this very treatment, knowing it would probably fail. Well it did fail.
At that time, I dispensed an orthotic where I increased the ability to plantarflex the first metatarsal by supporting the 1st metatarsal-cuneiform joint. This allowed for a more normal function of the first MPJ. This was very successful treatment that allowed the receiver to make his route maneuvers.
Jeffrey Trantalis, DPM, Delray Beach, FL
03/25/2024
RESPONSES/COMMENTS (CLINICAL)
From: Michael A. Uro, DPM
While I am very happy that Dr. Marino responded well to his carpal tunnel surgery, I wanted to point out that MLS laser treatments can help to minimize and in some cases totally alleviate the symptoms of carpal tunnel syndrome.
I have an MLS laser in my office. I was experiencing bilateral carpal tunnel syndrome. I treated myself using the laser, and after 3 to 4 treatments my symptoms subsided. I realize that not everyone has an MLS laser; however, if you can perhaps find a chiropractor or other practitioner who has one, I would recommend this treatment. Obviously, as podiatrists, we cannot treat carpal tunnel syndrome. Again I treated myself. The laser works on numerous nerve conditions on feet, such as tarsal tunnel syndrome and neuromas.
Michael A. Uro, DPM, Sacramento, CA
03/22/2024
RESPONSES/COMMENTS (CLINICAL)
From: Vince Marino, DPM
I recently (2 weeks ago) had bilateral carpal tunnel surgery done at one time. It took about 45 minutes under MAC. No post-op splints. I had minimal discomfort and was back in the office seeing patients (no palliative care) at 10 days post-op (included the weekend). I will be back doing surgery tomorrow at 17 days post-op.
My nerve studies were very abnormal and my fingertips constantly numb. Now I have no issues. I highly suggest you see a trained hand surgeon and talk about fixing the problem before it gets worse.
Vince Marino, DPM, Novato, CA
03/13/2024
RESPONSES/COMMENTS (CLINICAL) - PART 2B
From: Robert Kornfeld, DPM
I have spent more than 30 years treating chronic foot and ankle pain and have had many cases of “recalcitrant” PT tendinitis. Once you come out of the “next best treatment” mentality and focus on the patient, you will find answers. Functional medicine teaches you to examine the patient's total health landscape to uncover immune burdens and any epigenetic and genetic issues (SNPs) which will create inefficiency in repair pathways. These underlying mechanisms are managed prior to any treatment. Once you have up-leveled immune function, you can heal these chronic cases via regenerative medicine injection therapies. This is how every doctor should be practicing. I have loved my practice all these years.
Robert Kornfeld, DPM, NY, NY
03/13/2024
RESPONSES/COMMENTS (CLINICAL) - PART 2A
From: Jeff Root
Regarding the query about the treatment of recalcitrant "posterior tibial tendonitis", or what many would call posterior tibial tendon dysfunction (PTTD), I would like to share a few of my thoughts. The PM News subscriber stated that the patient wears "HOKA shoes and custom orthotics". The term "custom orthotics" simply implies that the devices were not prefabricated. In some cases, the lines between custom and prefabricated shoe inserts have been intentionally and unintentionally blurred. In addition, the term "custom orthotics" tells us little to nothing about the nature (i.e. design and properties) of the orthoses because there are hundreds if not thousands of types of custom orthotics and orthotic designs.
For example, what was the position of the joints of the foot, including the STJ, MTJ and 1st ray when the foot was casted or scanned? What were the specifications of the orthotic prescription? What lab techniques were used in creating...
Editor's note: Jeff Root's extended-length letter can be read here.
03/13/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1
From: David T Weiss, DPM
The most powerful way to manage DPN, (besides glycemic control,) is refraining from sugar (and carbohydrates) completely - especially after dinner. Sugar is extremely inflammatory. I have recommended liposomal glutathione (powerful antioxidant) as a supplement, along with L-methyl folate vitamins.
David T Weiss, DPM, Richmond, VA
02/27/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1 A
From: Robert Scott Steinberg, DPM
Not only are there too many schools, but the curriculum has not kept up to the standards for today's podiatric physicians and surgeons to become successful in practice. Colleges are not teaching the courses necessary for podiatrists to sit for the USMLE board exams, keeping the profession under the hallux of others. I suspect the first podiatric medicine college offering a better curriculum will get far more applicants. Let the race begin.
Robert Scott Steinberg, DPM, Schaumburg, IL
02/13/2024
RESPONSES/COMMENTS (CLINICAL)
From: Harold Koehler, DPM
I suggest running blood work to identify any other known causes of neuropathy. I had one patient recently that had neuropathy without any known predisposing conditions. When I ran a lab panel for potential systemic etiologies, he tested positive for high levels of mercury. Neither his primary doctor or the physiatrist could identify the source. The physiatrist suggested and referred him for chelation therapy, but the patient declined due to cost. I have no experience with a patient undergoing this treatment so I wonder if it would be effective. I did ask him about tuna consumption and it turns out he does eat an excessive amount; I think it was daily but I don't recall. Obviously he was told to stop.
Harold Koehler, DPM, Auburn Hills, MI
02/12/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1 B
From: Khurram Khan, DPM
Small fiber neuropathy (SFN) and large fiber neuropathy (LFN) represent two distinct categories of peripheral neuropathy, differentiated by the size of the nerve fibers they affect and the resultant symptoms and diagnostic approaches. SFN targets small myelinated Aδ fibers and unmyelinated C fibers, leading to symptoms like burning, tingling, and is diagnosed through hstory/clinical evaluation. LFN affects large myelinated fibers responsible for proprioception and vibration sensation, and with diagnosis typically achieved via physical exam and confirmed with nerve conduction studies and electromyography (EMG). The patient mentioned seems to have SFN. The causes of small fiber neuropathy (SFN) include:
Diabetes, autoimmune diseases (e.g., Sjögren’s syndrome, lupus, rheumatoid arthritis, celiac disease), infections (e.g., Lyme disease, HIV, hepatitis C), vitamin deficiencies (particularly vitamins B12, B6, and E), alcoholism, toxic exposures (e.g., chemotherapy drugs, heavy metals, industrial chemicals), hereditary disorders (e.g., hereditary sensory and autonomic neuropathies, Fabry disease), idiopathic (no identifiable cause), and finally metabolic disorders (e.g., thyroid dysfunction, amyloidosis)
Khurram Khan, DPM, Philadelphia, PA
02/12/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1 A
From: Lawrence Rubin, DPM, Bruce I Kaczander, DPM
The sensory dysfunction referred to by Dr. Teitelbaum is called "paresthesia." I have had some patients even complain of a feeling of "bugs running up and down my feet and legs" and similar sensations. Here is more information: Paresthesia: When to pin down a cause.
Lawrence Rubin, DPM, Las Vegas, NV
In my 42 years of practice, I saw patients daily whose neuropathic symptoms were spinal in origin (stenosis, L 4-5, S-1 disc)… it can oftentimes present initially as same, without the patient having current spinal symptoms. They also may have a history of same years ago.
Bruce I Kaczander, DPM, Southfield, MI
01/18/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1 B
From: Richard D Odom, DPM
I suspect the patient is a smoker. If so, his smoking is likely the etiology or cause of his lesions. The reason is because smoking/anxiety can cause these in areas of the body where there are an abundance of sweat glands, plantar foot & palms of hand. This increased moisture leads to some of the glands being over productive and can cause blockage of the surface of sweat gland. Farther production moisture is unable to escape from the gland, leading to increased hyperkeratotic build-up and pain from weight-bearing.
Stopping the smoking will reduce the hyperhydrosis, thus allowing the majority of the punctate lesions to most likely resolve over a 2-3 months period of time. The main point is to control the hyperhydrosis to minimize the re-occurrence of these painful lesions.
Richard D Odom, DPM (Retired), Decatur, GA
01/18/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1 A
From: Gary S Smith, DPM, Adrienne Sabin, DPM
I have had people improve greatly with Spenco insoles and spraying their feet daily with underarm antiperspirant spray.
Gary S Smith, DPM, Bradford, PA
Not knowing any other history of the patient, I suggest looking into Cowden’s syndrome as part of the differential diagnoses.
Adrienne Sabin, DPM, San Jose, CA
01/17/2024
RESPONSES/COMMENTS (CLINICAL)
From: Andrew Levy, DPM
My advice; unless your state specifically allows you to treat hands, refer your patient to a hand surgeon or dermatologist.
Andrew Levy, DPM (Retired), Jupiter, FL
12/09/2023
RESPONSES/COMMENTS (CLINICAL)
From: Chris Seuferling, DPM
The word “aching” brings to mind a couple of thoughts:
1. Chronic venous insufficiency. I know you said arterial status was intact, but what about veins? I’ve seen this cause aching pain even without obvious swelling or varicosities. Send for venous mapping/testing. Try compression stockings.
2. Any alcohol use/abuse? I’ve seen this cause generalized leg aching symptoms, particularly at night.
Keep us updated.
Chris Seuferling, DPM, Portland, OR
12/08/2023
RESPONSES/COMMENTS (CLINICAL)
From: Stephen Leonard, DPM, Chris Seuferling, DPM
I would be suspicious of a tarsal coalition. Order a CT scan of bilateral feet and ankles to rule it out.
Stephen Leonard, DPM, Spring Hill, FL
Is there any history of trauma, of any type, related to onset of symptoms? Any significant findings with family history? I would be interested to know how he responds to gabapentin. Depending on the response to the two above inquiries, I would consider a second opinion with another neurologist.
Stephen Musser, DPM, Cleveland, OH
10/31/2023
RESPONSES/COMMENTS (CLINICAL)
From: Robert G. Smith, DPM, MSc, RPh
First, I would like to thank Dr. Kravitz for his excellent, insightful, observational, narrative. The worldwide substance abuse crisis continues. It is inescapable not to acknowledge the contaminates and poisons used to cut substances of abuse. These poisons have adverse effects to the integumentary system to those suffering from substance use disorder. Secondly, dermatological manifestations and sequelae of opioids, cannabis, cocaine, crocodile, methamphetamine, alcohol, and of course xylazine have presented to practicing podiatric physicians.
Lastly, I agree with Dr. Kravitz that the addition of a pain management/substance use disorder rotation will benefit podiatric residents, their patients, and the podiatric profession. For that reason, I continue my research centered on “following the opioid settlement money” by contacting each state attorney general to inquire: “What are their plans for the settlement money?” I have only received a 24% response rate. I continue to send emails and calls to increase this response rate. As a private citizen and the founder of my 501(c)(3) non-profit educational company “Studying Opioid Harm”, I am advocating that podiatric residency programs receive a fair portion of these funds for a pain management/substance use disorder rotation.
Robert G. Smith, DPM, MSc, RPh, Ormond Beach, FL
10/30/2023
RESPONSES/COMMENTS (CLINICAL)
RE: Xylazine-Laced IV Injections and Advanced Skin Ulcers
From: Steven Kravitz, DPM
This past spring, President Biden recognized the urgency of needed medical awareness for skin ulcers that are extremely aggressive from injections laced with xylazine by IV drug users. This is a large animal sedative used by veterinarians. When injected into human skin, it causes excessive necrosis with very aggressive ulcers, and can lead to complete skin loss from the knee down through the ankle. Systemically it is very dangerous causing a severe decrease in blood pressure and potential death. It is not approved by the FDA for human use but has increasing usage and availability by those using IV drugs, illegally, such as heroin, etc. Therefore the ulcer related to xylazine has become more commonly seen.
The ulcer is largely unrecognized by the medical community and often misdiagnosed as a pyogenic granuloma, pressure ulcer, and...
Editor's note: Dr. Kravitz's extended-length letter appears here.
10/18/2023
RESPONSES/COMMENTS (CLINICAL)
RE: Proper Blade for Debridement of Calluses (Ivar E. Roth DPM, MPH)
From: Stephen Peslar, BSc, DCh
I concur with Dr. Roth. Careful scalpel technique is superior to using a dermal curette. 40 years ago, I learned how to enucleate IPKs. I use a Miltex #3 handle and a Swann-Morton #15 blade. For calluses, I use a #10 Swann-Morton blade. From time to time, I do get bleeding points; they are treated with a topical antibiotic and an appropriate sterile dressing.
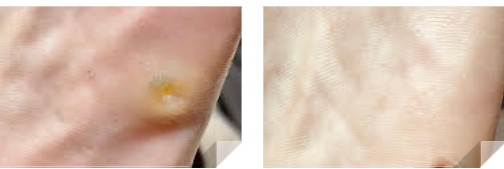 |
Debridement of Calluses with Swann-Morton blade |
This was a recent case.
Stephen Peslar, BSc, DCh, Toronto, Ontario, Canada
10/17/2023
RESPONSES/COMMENTS (CLINICAL)
From: Stanley Beekman, DPM
In the rare cases of plantar fasciitis which were non-responsive to conservative care, I would get an MRI which would show: bone marrow edema, mucoid degeneration of the plantar fascia, and partial tearing. The procedure I would use removes the calcaneal spur to treat the bone marrow edema, then I would inject the platelet gel (spun down at the hospital) into the plantar fascia.
The initial mistake I made was not immobilizing the patient post-op. I found that 3 days off-weight-bearing and then the use of a CAM walker for a month was required.
Stanley Beekman, DPM (Retired), Avon Lake, OH
|
| |

|
|
|