





|

|
|
|

|
Search
05/12/2022
RESPONSES/COMMENTS (CLINICAL CASES)
RE: Retronychia, a Rarely Diagnosed Nail Disorder
From: Leonard A. Levy, DPM, MPH
A presentation at the annual meeting of the 2022 American Academy of Dermatology on retronychia, a nail disorder of the toes, was made by Phoebe Rich, MD, director of the Nail Disorders Clinic at Oregon Health & Science University, Portland. The disorder was described as the growth of new nail under prior nail growth. Dr. Rich states that antifungals and antibiotics, even for years, have no place in treating this condition since infection is not commonly involved in retronychia. Microtrauma typically serves as a trigger to retronychia. Dancing, high heels, steel toed shoes and other sources of trauma have been implicated. Some but not all patients have abnormal function of the nail bed, according to Rich, increasing susceptibility to retronychia. Injury separates the existing nail from the matrix and nail bed so that newly formed nail begins to grow under the nail, pushing out the old nail.
 |
Retronychia |
Even when the nail is removed and regrowth appears normal at the end of a year, patients with very short nails cannot count on a cure. Slow nail growth may result in recurrence in 2-3 years. Rich remarks that there is no diagnosis by histopathology, so it cannot be confirmed by biopsy. Conservative treatments, including topical and intralesional steroids, have been effective in mild cases to more invasive and effective surgical avulsion. She states that only 50% of yellow thickened nails are onychomycosis, resulting in a plethora of patients with retronychia who are misdiagnosed.
Leonard A. Levy, DPM, MPH, Ft. Lauderdale, FL
Other messages in this thread:
05/13/2022
RESPONSES/COMMENTS (CLINICAL CASES)
From: George Jacobson, DPM
Thank you Dr. Levy for that description. I have never heard or the term retronychia but we have all seen this occur throughout our careers. In some cases of trauma, the new nail plate does not adhere to the nail bed either, even without onychomycoses present.
There is no ICD-10 for this condition. I have used onycholysis (L60.1) as the description and describe the new underlying second nail plate.
George Jacobson, DPM, Hollywood, FL
07/07/2021
RESPONSES/COMMENTS (CLINICAL CASES)
RE: Plantar Purpura Due to Cardiac Myxoma Embolism
From: Leonard A. Levy, DPM, MPH
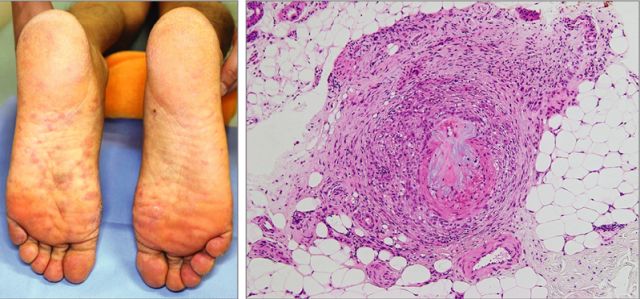
After experiencing painful purpura on the volar aspect of the left hand that resolved after a few days, a 52-year-old man had a relapse consisting of purpura on the left plantar area followed by the onset of left hemiplegia and dysarthria. A biopsy of the purpura of the left plantar lesion was conducted revealing subcutaneous intracapillary occlusion positively stained with Alcian blue and calretinin.
|
Clinical image of soles, hematoxylin-eosin stain |
Computed tomography and echocardiography detected a right cerebral infarction and a 23 mm mass in the left atrium which was resected, leading to a diagnosis of cardiac myxoma and the conclusion that the painful plantar purpura was due to cardiac myxoma. (Yoshihito, O, et al. Painful Palmar and Plantar Purpura, JAMA Dermatol. Online June 30, 2021)
Leonard A. Levy, DPM, MPH, Ft. Lauderdale, FL
03/11/2021
RESPONSES/COMMENTS (CLINICAL CASES)
RE: Painful Hand and Foot Plaques
From: Leonard A. Levy, DPM, MPH
A 56-year-old man presented to the Dermatology Clinic of the University of New Mexico School of Medicine with painful plaques he had for years on his hands and feet. He worked in construction and attributed the pain in his hands and feet (7/10) as the causes of the problem. He had tried acitretin to treat the plaques but stopped when his skin turned red and became dry and itchy. A diagnosis of hand and foot psoriasis with classic thick scale and erythema on his palms and soles was concluded. Additionally, on the sole toward the heel, he had hyperpigmented macules called mahogany spots, another hallmark of psoriasis. Pitting and distal onycholysis were also visible on his right ring finger.
 |
Painful Hand and Foot Plaques |
While UVA or narrowband UVB light therapy is a treatment option, it requires 3 visits per week, not conducive to his work schedule and daily activities. Acitretin was prescribed to decrease the abnormal proliferation of keratinocytes; however, he experienced dry skin and itching. Initially, however, he was treated with topical calcipotriene (a vitamin D derivative) and clobetasol (high-potency topical steroid) without adequate improvement. In addition, screening lab tests showed elevated liver enzymes, precluding treatment with methotrexate (and acitretin, which he’d received previously). He was started on apremilast, which can can cause diarrhea, depression, nausea, and headache. But other than some loose stools, he tolerated apremilast well and showed significant improvement in his psoriasis at a 3-month follow-up visit. (Painful hand and foot plaques, J. Fam Prac. January 2021, 70(1) .
Leonard A. Levy, DPM, MPH, Ft. Lauderdale, FL
|
| |

|
|
|







