





|

|
|
|

|
Search
09/09/2009
QUERIES - CLINICAL
Query: Calcaneal Ostectomy and Decreased Fat Pad
The x-ray shown is that of the left foot of a 70 y/o diabetic female patient who underwent a partial calcanectomy 2 years ago, secondary to osteomyelitis. The present issue is loss of fat pad, pre-ulcerative lesion, and significant pain, plantar calcaneus. Conservative measures have been exhausted, including custom accommodative inserts, shoes, bracing, and pain management. Minimal relief has been achieved. She's not interested in further conservative treatment. She understands the risks of surgery, but wishes to pursue surgical intervention. Her pain is severe enough that she is contemplating amputation, if all else fails.
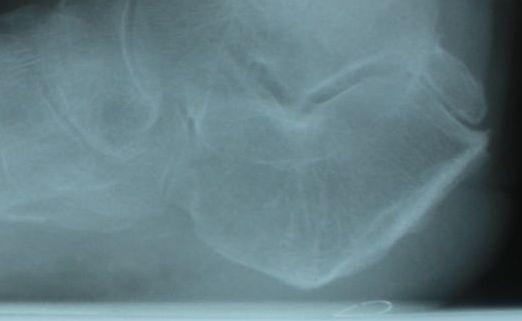 |
Loss of Fat Pad, Post Partial Calcanectomy |
I'm planning on contouring the plantar calcaneus, but I am wondering what my options are to address the loss of fat pad? Does anyone have any experience or success with autologous fat transfer, GraftJacket, tissue augmentation, or other modalities which would be effective in this setting?
Chris Seuferling, DPM, Portland, OR
Other messages in this thread:
06/18/2012
QUERIES - CLINICAL
Query: Is This MTPJ Salvageable?
This 56 year old female with long standing HAV would like to fit in shoes comfortably and have her foot look better. I am considering CBWO and a fusion of the 1st MTPJ. I do not think there is enough room for the metatarsal to move at the base to allow closing the IM without metatarsal work. Am I wrong?
 |
Is this 1st MTPJ salvageable? |
Some colleagues are recommending other procedures to "save the joint". My concern is finding cartilage that is healthy.
Alan Berman, DPM, Carmel, NY
01/23/2012
QUERIES - CLINICAL
Query: Integrative Nerve Blocks
I have had some patients come into my office relating that their primary care doctors are sending them to pain clinics that advertise integrative pain blocks for diabetic neuropathy. Apparently, they get weekly or sometimes bi-weekly ankle blocks, along with what they call 30-minute electronic signal treatments. They go weekly for 6-8 weeks. Some patients have come back with decent results, yet some have had no improvement. Does anyone have knowledge whether this is a viable treatment plan?
Saleem Ahmed, DPM, Lexington, KY
07/16/2010
QUERIES - CLINICAL
Query: Recurrent Nodular Tumors I have a female patient who is moderately obese, 50 years of age, diabetic type I x 20 years and has SLE. I have removed several large (3-4cm) subcutaneous masses from her forefoot that have recurred on multiple occasions in different but adjacent locations. On each dissection the pathology report is the same. It reads as follows: "Fat necrosis with surrounding fibrosis, adjacent hemosiderin laden macrophages and vascular proliferation with congestion. No diagnostic features of malignancy.” The cystic-like nodules are semi-demarcated from surrounding tissue, but very adherent to deep fascial tissue, rubbery texture and whitish-grey in appearance. The patient and I are both frustrated with recurrences over the years. Any comments or suggestions? Angelo J. Bigelli, DPM, North Providence, RI, toedocri@aol.com
11/16/2009
QUERIES - CLINICAL
Queries: Platelet-Rich Plasma I would like to know about results on PRP injections. Can they be used as a first line treatment? Does it have to be done in the office or in the hospital? How many injections can the patient have? What is the protocol? I understand that the 50ml of the patient’s blood must be taken and spun to get 3ml. Jason M. Grossman, DPM, Old Bridge, NJ
08/31/2009
QUERIES - CLINICAL
Query: Ascending Cellulitis and Antibiotics I had a patient who presented to my office for the first time with c/o athlete’s foot infection after working outside all day. He was at his doctor's office the day before. On presentation, the patient had edema, redness to the foot with interdigital macerations, and ascending cellulitis up the leg to the level of the knee. I advised him to go to the ER and get admitted for IV antibiotics the same day. Patient went and was given one dose of IV and sent home with "stronger" PO antibiotic. Is there a time or situation when a patient with ascending cellulitis up the leg does not need to be treated with more than one dose of IV antibiotics? Vilayvanh Sysounthone, DPM, Wayne, NJ
07/20/2009
QUERIES - CLINICAL
Query: Lipoma or Liposarcoma I have a patient who has a 3 inch x 3 inch soft tissue subcutaneous tumor on the medial right heel. X-rays negative. Past medical and surgical history is non-contributory. MRI report said lipoma or liposarcoma due to septations seen. I am planning an intra-operative biopsy with frozen section. If it is a lipoma, I will remove it. If it is a liposarcoma, should I excise the tumor and refer to surgical oncologist or just sew up at that point and refer to a surgical oncologist? Richard Silverstein, DPM, Havre de Grace, MD
|
| |

|
|
|







