





|

|
|
|

|
Search
11/23/2021
RESPONSES/COMMENTS (NON-CLINICAL)
RE: Clinical Quality Measures for Podiatry
From: Craig Herman, DPM
I am currently trying to develop or discover clinical quality measures for our profession. The two obvious measures are diabetic foot exams and fall prevention. However, I am looking to develop new measures dealing with positive clinical outcomes and possibly incorporating social determinates of health in patients under the age of 65, and non-diabetics. Any suggestions will be appreciated,
Craig Herman, DPM, Jamaica, NY
Other messages in this thread:
04/24/2025
RESPONSES/COMMENTS (NON-CLINICAL)
From: Judd Davis, DPM
I agree with what others have said about the abuse and overuse of these skin graft substitutes. The vast majority of wound patients do not need these to heal. I was approached by a rep from a very large and publicly-traded medical product company to start using these grafts on my patients. He told me a tale of their top performer, a DPM in New York who did a lot of nursing home and wound care work, who had used about $20 million of their product in the last year alone. When I related that seemed fraudulent to me, the rep suggested that an offshore account could be set up to hide the money so it would be untouchable in the event that any of the treatment was determined fraudulent. I advised him that I was not interested in such schemes.
A few months passed and a patient came to my office with non-healing diabetic foot ulcers. Another provider in town had applied a series of 4-5 grafts on weekly intervals, costing over $100,000! The wounds did not heal. I am amazed that CMS has not completely shut down all use of these grafts with this type of abuse occurring.
Judd Davis, DPM, Colorado Springs, CO
04/23/2025
RESPONSES/COMMENTS (NON-CLINICAL) -PART 2 A
From: Allen M. Jacobs, DPM
The increasing cost of wound care, including the employment of skin graft substitutes, is not a podiatry centric problem. Many factors, such as an aging population, the rise in disorders with which wounds are associated (e.g.: diabetes, PAD, venous disease) have continued to drive the need for wound care. The failure of insurers to provide reasonable or in fact any payment for preventive care is a factor. Socioeconomic issues such as patient access, patient education, patient financial concerns are factors.
The expense associated with dressings, skin graft substitutes, de-facto referral of patient referrals to wound care centers, contribute to the problem. With specific reference to skin graft substitutes, Dr. Geistler notes in PM News that in his experience, skin graft substitutes are not required for the management of most wounds. There are over 350 "skin graft substitutes" available world-wide. Many are extraordinarily expensive, with little...
Editor's note: Dr. Jacobs' extended-length letter can be read here.
04/23/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 2 B
From: Ivar E. Roth DPM, MPH
My highest accolades for Dr. Geistler opinions on the overuse and abuse of grafts being used in podiatry. He is right on, and I am proud to call him a true professional. I agree... throw the book at our fellow practitioners who are just milking the system for the dollars and really NOT helping the patients at all.
Ivar E. Roth DPM, MPH, Newport Beach, CA
04/23/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 1
From: James Hatfield, DPM
The post by Louis Profeta, MD is excellent and should be required reading by all residents, students, and applicants. I'm so tired of hearing all the whining going on about our profession. We have an excellent future and waste too much time obsessing about our degree. Get a life!
James Hatfield, DPM, Encinitas, CA
04/21/2025
RESPONSES/COMMENTS (NON-CLINICAL)
RE: Acellular Grafts
From: Perry K. Geistler, DPM
I have been in practice for 33 years. I do work in my private office as well as on call at our hospital and see patients in our hospital wound care center. I went over my statistics for last year and I averaged seeing 32 ulcers a week for 48 weeks, not individual patients but ulcers. I have found it the gross exception to have to use a graft to heal anything. I certainly use grafts but when I went over my numbers, I used a graft on 4.8% of my patients last year.
Most people who have ulcers are going to heal with using the basic paradigms; such as, off-loading, establishing circulation, taking care of systemic illnesses or contributing morbidities, surgically removing...
Editor's note: Dr. Geistler's extended-length letter can be read here.
04/19/2025
RESPONSES/COMMENTS (NON-CLINICAL)
RE: Practice Dissatisfaction
From: Robert Kornfeld, DPM
Over the past 38 years, I have worked with many doctors in the field of functional medicine and regenerative medicine. And we are a very happy and satisfied group of doctors. About 2 1/2 years ago, when I became very active on LinkedIn, I became aware of the stark reality of most doctors out there. Unhappiness, malcontent, frustration, disappointment, anxiety, depression, burnout, anger and high levels of stress have caused most to be really miserable in practice. And I'm not only speaking about podiatrists. It's universal among all doctors.
And when they share why, that is universal too. It is a combination of the low fees, unpredictable payments, administrative burdens, enormously high volume of patients they have to treat, or unscrupulous and demanding employers who put them under constant stress and don't pay them fairly. Yet, for some reason, it is the pink elephant in the room. Does the next new surgical approach or instrument really matter if you are miserable? Is the next new modality really...
Editor's note: Dr. Kornfeld's extended-length letter can be read here.
04/14/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 2
From: Rod Tomczak, DPM, MD, EdD
I really want to thank Dr. Secord for his German compound word idioms. It plays precisely into the completion of defining podiatry. When I was 16, I still was fluent in German, attending a boarding school near Aachen. I still dream in German once or twice a month, but nowhere like it used to be. As a lone monk chants at the burial of as pope, “Tempus fugit, memoria mortem.” Time flies, remember death.
For quite some time, we have defined ourselves as the primary care givers of feet, especially for what we identify as sick feet. Let’s be honest, most of us don’t do reconstructive surgery on feet with multiple complex deformities and use external fixation. Orthopedic foot and ankle care givers don’t have time during their one-year fellowship to learn what we learn in seven years. If you want to make it a binary distinction, we take care of sick feet that have sometimes...
Editor's note: Dr. Tomczak's extended-length letter can be read here.
04/14/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 1
RE: Podiatry’s Identity Crisis
From: Arden Smith, DPM
Background: this is my third winter since retiring and snow-birding. Both my former partner and I are both double boarded and we were lucky enough to have developed a very early niche in the medical and surgical treatment of the high-risk diabetic foot and limb salvage through having a satellite office within a large endocrine practice, beginning in the mid-1980s. This was something that we had very little training for and learned by the seat of our pants and attending diabetic foot conferences. We started out asking a friendly vascular surgeon if we could assist on referred cases and over a relatively short period of time, started asking him if he wanted to assist us; and then eventually stopped asking, other than the vascular consult. We also had a large volume general podiatry practice that was somewhat surgically oriented. We would see multiple generations in families.
Our general practice was a neighborhood practice in a middle class area, and our diabetic practice was a referral hub between two...
Editor's note: Dr. Smith's extended-length letter can be read here.
04/10/2025
RESPONSES/COMMENTS (NON-CLINICAL)
From: Bill March, DPM
Thanks to Dr. Secord for his enlightening, educational, and entertaining response to Dr. Tomczak's frequent lengthy, erudite missives. Only took an extra 10 minutes to research, educate and enlighten myself using Dr. Google. Very impressive! Had Latin and French in HS, no help. German may have. Recently retired after 40 phenomenal, fabulous, and VERY satisfying years helping people with their feet and listening to their problems. I could not have wished for a better life or profession.
I was considering discontinuing PM News, but the variety and quality of the letters will keep me reading. Much better than politics! Thanks, fellows. Keep smiling and enjoy something every day.
Bill March, DPM, Cherry Hill, NJ
04/09/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 2
From: David Secord, DPM
Once again, Dr. Tomczak helps focus upon the pivotal point in the progression of our fate. That he does so while being able to throw in a little modus tollens Aristolean syllogistic logic is that much more entertaining. It had been a while since I’d seen the term portmanteau, so kudos!
His description of our struggles to define ourselves before we can define what we do and who we are as a profession to the lay public as a synecdoche or metonymy rings true. Dr. Tomczak does a wonderful job in his musings as a erziehungsroman of sorts. We are truly, as a profession, writing a bildungsroman as we go. Hopefully, the story will end as a victory and not a tragedy. Change is inevitable. Our indecision to initiate and continue the journey is not encouraging.
David Secord, DPM, McAllen, TX
04/09/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 1
RE: Podiatry Salaries vs. Nurse Salaries from Becker's Hospital Review
From: Steven D Epstein, DPM
Certified registered nurse anesthetists (CRNAs) make more than most of us do. An RN makes this after only four years of undergraduate education. And this doesn't preclude them from going into advanced practice; in fact, experience as a "mere" RN is usually required to be accepted for advanced practice training. Failing to be accepted for that consigns one to a miserable six figure salary career.
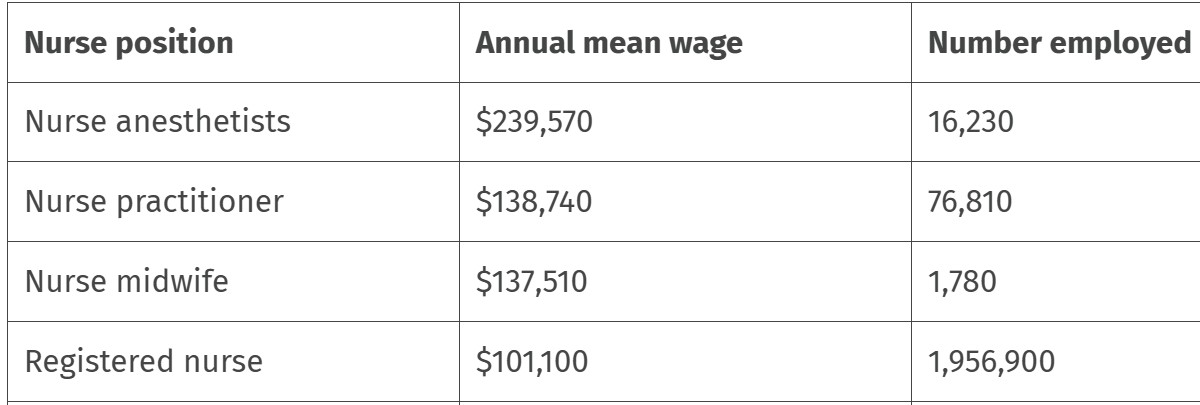 |
Nurse's Salaries (Source: Becker's Hospital Review) |
This kind of info is now freely available for high school and college students to see. Is it any wonder that smaller numbers of students are choosing podiatry as a career?
Steven D Epstein, DPM (retired), Lebanon, PA
04/07/2025
RESPONSES/COMMENTS (NON-CLINICAL)
From Paul Kesselman, DPM
A recent Medical Economics and Wounds email blast provided a thorough discussion regarding physician reluctance to seek help for symptoms related to burnout. I urge anyone in any specialty to read these articles and urgently seek help if they have any symptoms detailed in these recent publications and their referenced articles.
Paul Kesselman, DPM, Oceanside, NY
04/03/2025
RESPONSES/COMMENTS (NON-CLINICAL)
From: Elliot Udell, DPM
I get that your experience of Landmark was quite different from what participants are experiencing in 2025. The course I am taking is run by a practicing psychiatrist who dedicates many hours from his private practice to work with people under the Landmark banner. Be that as it may, I have heard some of the stories from people who took Landmark training 30 years ago. It was quite rigid in those days, and I don't know if I would have been able to get through it way back then.
So, I am inviting you and others to come online on April 8th at 7 PM and experience the new Landmark training and determine if it will help you in your life and in your podiatric practices. There is no charge for coming in as a guest and there is no pressure to take any of their 60 courses.
Elliot Udell, DPM, Hicksville, NY
04/02/2025
RESPONSES/COMMENTS (NON-CLINICAL)
From: Joel Lang, DPM
For those who are unfamiliar with Landmark Worldwide, it is a spin-off from the previous "The Forum" which was a spin-off from the previous "EST - Ehrhart Seminar Training". I took The Forum back in the ‘70 or ‘80s and visited one "guest session" of Landmark Worldwide some 20 or so years later, invited by a neighbor. Recruitment seemed to be the main purpose of bringing guests.
The seminars themselves, were intense at the time, everyone seated in person in tight rows, in straight back chairs, shoulder to shoulder for extended hours - like early morning to nearly midnight. No notebooks, no phones, no pagers, no tables, just seated in tight quarters, with limited "allowed" breaks for bathrooms. Seating was so tight that it was very difficult to leave and return. Leaving on your own for breaks was severely discouraged and you were required to sit in the same seat, next to the same people, for the duration of all sessions. It provided some good insights, but it could be very intense.
It was also very high pressure, always encouraging current members to bring in new members. Of course, the special “guest sessions" were much shorter. It is only through finding new bodies that seemed necessary for the organization's survival. The new members brought were subject to high pressure tactics to join. It also seemed cultish to me. I am not familiar with this new online version, probably dictated by Covid concerns. It could be entirely different since it does provide some physical separation and may have changed, but I suggest "guests" be cautious.
Joel Lang, DPM, (retired), Cheverly, MD
03/31/2025
RESPONSES/COMMENTS (NON-CLINICAL)
From: Elliot Udell, DPM
Dr. Kesselman is correct. Burnout can affect anyone working in any high-intensity medical profession. Stress comes with the territory when you are taking care of sick people, especially in the current environment where there is pressure on healthcare providers to work harder and faster.
I am currently enrolled in a ten-session program that helps individuals from all professions manage life's stressors. It's called Landmark Worldwide. On April 8th at our final Zoom session, I can bring guests for free to check out the program. If anyone is interested, contact me directly and I'll send you a formal invitation.
Elliot Udell, DPM, Hicksville, NY
03/27/2025
RESPONSES/COMMENTS (NON-CLINICAL)
RE: LEAP Alliance and NCQA
From: Lawrence Rubin, DPM
A major obstacle to achieving diabetes amputation prevention goals is a general lack of insurance coverage for preventive foot screening examinations - this in spite of the fact that early detection and prompt treatment of diabetic peripheral neuropathy and peripheral artery disease saves limbs and lives. The goal is to provide insurance coverage for performing a thorough diabetes patient foot screening exam at least once a year. Payers would need provider compliance with a Healthcare Effectiveness Data and Information Set (HEDIS) measure - and no such measure exists.
HEDIS measures are performance measures developed by the National Committee for Quality Assurance (NCQA) to measure, report, and compare the quality of care provided by health plans. With hopes of overcoming this obstacle, the LEAP Alliance is advancing an initiative to implement its proposed diabetes patient preventive foot examination measure. We have been successful in scheduling a meeting with NCQA. Its administrators have expressed interest, and hopefully this meeting will be productive.
Lawrence Rubin, DPM, Las Vegas, NV
02/28/2025
RESPONSES/COMMENTS (NON-CLINICAL)
From: Richard M. Maleski, DPM, RPh
I'm glad to see someone else is interested in seeing the DPM's role go from cutting nails to overseeing the management and treatment of nail pathology. I've opined in this forum a few times now that we should not be spending our time on the physical practice of cutting nails. About 30 years ago, I spoke with the Executive Director of our state society (PPMA), Michael Davis, about the possibility of having podiatric assistants cutting nails and still being able to bill for that. At that time, he told me that podiatrists were not legally able to supervise such activity in Pennsylvania, let alone bill insurance for it.
When I asked how difficult would it be to change that, he said that it would probably have to involve state legislative changes, which would be very difficult. I did speak with a Board member also, a DPM, and he felt that there would be very strong resistance from the podiatric community. Most DPMs were very content to ...
Editor's Note: Dr. Maleski's extended-length letter can be read here.
02/27/2025
RESPONSES/COMMENTS (NON-CLINICAL)
From: H. David Gottlieb, DPM
Change is constant in life and in podiatry. The APMA used to be the APA, and before that, NAP. The degree used to be DSC (and PodD) before DPM. Podiatry schools in the early '80s had as their mission "to prepare graduates for practice.'' Now, their mission is to "prepare graduates for residency." Many states did not require residencies for a license. Now most do, and I expect very few, if any, require only a one-year residency.
Providers on this forum complain incessantly that the APMA is not addressing the current "crisis"' facing our profession… that they need to do something to be more aggressive… that the current staff needs to "wake up''. So change is being made. First, someone with an MBA is hired to lead the organization - someone with a fresh perspective who can evaluate APMA as a business, which it is. After assessing the business of APMA and determining what "needs" need to be met in order to be successful, appropriate changes are being made to accomplish those goals. APMA is no longer doing business as usual.
So, as I see it, APMA is first being criticized for not making changes to address the current crisis but when APMA starts to make changes to meet the challenges facing this profession, TODAY they get criticized. Give me a break. Change must be made. Change IS being made.
H. David Gottlieb, DPM, Baltimore, MD
02/26/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 2B
From: Ivar E. Roth, DPM, MPH
Dr. Whelan is correct. Let’s take control of this situation. The writing is clearly on the wall; we as a profession have to move, and move fast to make sure we are in charge of any change. The students graduating today are not interested in routine care. It is sadly now a fact. Also, we have to lose the limited license aspect of our profession. We are so well trained, but can do less than a PA, nurse, or many other allied professionals.
The time is now. Who will lead the charge is dependent on our leaders, but the time has come.
Ivar E. Roth, DPM, MPH, Newport Beach, CA
02/26/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 2A
From: Thomas A. Graziano, DPM, MD
Dr. Whelan brings up some salient points when addressing the concerns over the future of podiatric medicine. Many years ago, the foot was neglected by the medical community and podiatry came into its own by filling that void. The current requirement for EVERY podiatry school graduate to complete a 3-year surgical residency has fostered the neglect of routine foot care. And now that void appears to be filled by nurses or non-podiatric ancillary staff. History may be repeating itself.
In 41 years in practice, I've seen the gradual decline in the public's perception and the insurance industry's devaluation of healthcare professionals. We are no longer perceived as doctors. We are now looked at by the insurance industry and to some degree by the public merely as "providers."
The recent survey on this forum demonstrating that if given the choice, over 43% would prefer a career path in osteopathic medicine is not at all surprising. Let's address the elephant in the room. A good friend of mine whose son just completed a DO family practice residency accepted an offer of 350K/annum as a hospitalist. And this for an 18 day/month work schedule. Perhaps the survey results and paucity of podiatry school applications might have something to do with the disparity between podiatry and osteopathic medicine.
Whether one agrees or not as to why the profession of podiatric medicine is at a crossroads right now, there's no doubt the writing is on the wall. 300 applications to all the podiatry schools sends a clear message. Dr. Whelan's comments may not only be insightful but may be a necessity in the very near future.
Thomas A. Graziano, DPM, MD, Clifton, NJ
02/26/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 1
From: Lawrence Rubin, DPM
Along with others posting, I was saddened to hear that APMA has fired two very qualified and seasoned health policy employees. I hope there is justification for this, since national health policies having to do with health insurance reimbursement are changing dramatically with the advancement of the Medicare led value-based care payment model. APMA health policy employees should be thinking forward and hard at work developing ways and means to help its members transition to value-based care now, as it is already moving forward and is considered the future of healthcare to be fully implemented in 2030.
Value-based care offers numerous benefits for both patients and providers. These benefits include improved patient outcomes, greater physician satisfaction, and a more sustainable financial model by focusing on quality of care rather than just volume of services delivered. It also offers financial rewards for those podiatrists who will collaborate in providing lower extremity chronic disease prevention services.
APMA members who delay the transition due to lack of information and guidance could potentially be missing opportunities for better patient care and could put their practices at a competitive disadvantage. Hopefully, this was considered when the decision to fire these employees was made.
Lawrence Rubin, DPM, Las Vegas, NV
02/25/2025
RESPONSES/COMMENTS (NON-CLINICAL) -- PART 2
RE: Source for Injectable Alcohol
From: Louis Cappa, DPM
I found a compounding pharmacy that sells injectable alcohol for neuromas...Compounded Solutions in pharmacy in Monroe, CT
Louis Cappa, DPM, New Windsor, NY
02/25/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 4
RE: Redefining Roles in Podiatric Care: Exploring the Potential for a Standardized Foot Care Assistant Model
From: James H Whelan, DPM
The landscape of foot and ankle care is evolving. With an aging population, a growing number of patients with diabetes, and shifts in podiatric training emphasizing surgical intervention, there is an increasing need to ensure continued access to high-quality foot care while reinforcing the role of podiatric physicians as the foremost experts in foot and ankle health. A topic of growing discussion within the profession is the expansion of routine foot care services provided by non-podiatric healthcare professionals. While this raises concerns about scope of practice, it also presents an opportunity to explore structured, podiatrist-led models that enhance patient care and optimize the efficiency of podiatric practices.
One potential solution is for professional organizations such as APMA and ACFAS to evaluate the feasibility of developing a standardized Foot Care Assistant (FCA) role—a structured position within podiatric practices that allows trained professionals to...
Editor's note: Dr. Whelan's extended-length letter can be read here.
02/25/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 3
From: Rod Tomczak, DPM, MD, EdD
There are now 37 osteopathic schools in the United States, meaning more seats. There are 158 MD schools in the U.S. which are not increasing in numbers or seats. LCME and AAMC limit the number of seats at each medical school and there is no increase in the foreseeable future. Acceptance to a Caribbean medical school is a given, but passing USMLE is a crap shoot. DOs take the same USMLE licensing exams as MDs and match into historically allopathic residencies.
The difficult part of the plan will be extending the DPM residency funding to include DOs with a one-year general internship that has been allocated for DPMs. If, however, there are no DPMs, or only a few pure DPMs, there will be money available. Remember, the new DO foot and ankle provider must learn everything about the foot and ankle in two years of residency training. Foot and ankle orthopedic fellows do it in one year.
It will be easier for a future non-DPM foot care specialist to get accepted into a DO school. I take umbrage with the conceptualization of DOs as intrinsically different than MDs. DOs and MDs use the same textbooks and take the same USMLE exam for licensing and match into the same residencies. Some MD schools are combined with a DO school. How many strict DO hospitals are you aware of? Historically, DOs had to serve a one-year internship in a DO hospital to gain privileges at a DO hospital. That concept went the way of the lamplighter, milkman, and DO hospital. I see these foot care specialists being certified by a single board titled something like the American Board of Foot and Ankle Medical Specialties. All the other certifications will be superfluous and obsolete. Time to come together.
Rod Tomczak, DPM, MD, EdD, Columbus, OH
02/25/2025
RESPONSES/COMMENTS (NON-CLINICAL) - PART 1
RE: Shocked and Saddened
From: Mark Block, DPM
On February 21st, out of the blue, I, along with the APMA membership, was informed of significant changes within the Association. It appears that APMA has decided to undergo a major restructuring.
Having been a long-standing member since my time as a student, I recognize that while other podiatric entities contribute meaningfully to our profession, APMA along with other missions serve as a unifying voice. Its ability to lobby and advance legislative initiatives is essential to the profession’s strength and future. I have come to appreciate that the Association’s long-term viability must be ensured. Should APMA cease to exist, it would leave a tremendous void with serious negative ramifications...
Editor's note: Dr. Block's extended-length letter can be read here.
|
| |

|
|
|







