





|

|
|
|

|
Search
12/21/2016
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Don Peacock, DPM
I agree with most of the post Dr. Rosenblatt has eloquently described. It is essential that surgeons address gastrocnemius equinus when the deformity presents. It’s equally vital that we incorporate bio-mechanical exams in our surgical endeavors.
I do take some exception with his conclusion that performing a MIS bunion correction without fixation will always lead to second metatarsal transfer pain. The research in this area contradicts this statement. Non-fixated first metatarsal osteotomies such as the landmark research Dr. Dale Austin gave us is a...
Editor's note: Dr. Peacock's extended-length letter can be read here.
Other messages in this thread:
05/19/2025
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: David Secord, DPM
Some years back, I was treating a border patrol agent who caught a Mesquite tree thorn in her thumb. She was “treated” at the E.R. and was still having problems. Why? Upon examination, the thumb was about twice the expected diameter—indicating that a foreign body was still present—and the incision made was closed with 2.0 Ethibond. In this case, an examination of the procedure revealed that this was not done by a doctor, nor a PA. Not done by a NP either. This atrocity was committed by an MA. They had a medical assistant (who, rather obviously has zero qualifications or permission to perform a surgical procedure on anyone) inject, incise, poke around, not find, and suture with totally inappropriate material a foreign body procedure.
I don’t know if this relates to the hernia procedure, but one never knows. I recently inherited a patient post-hallux amputation procedure who was told (and given written instructions) that he could immediately start bathing the site, still sporting the nylon sutures. I don’t know if I’ve missed something new, but the “go ahead and bathe immediately post-op” idea isn’t supported by any science and is strongly opposed as far as I’m aware. There is some questionable stuff out there.
David Secord, DPM, McAllen, TX
04/24/2025
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: David T. Weiss, DPM
The effective concentration of dextrose is 50% (hyperosmolar).
Mechanism of Action of Dextrose:
1. Localized Inflammatory Response Dextrose solutions (typically hyperosmolar) act as an osmotic irritant when injected into entheses, ligaments, tendons, or joint capsules. This mild irritation triggers a controlled, localized inflammatory response.
2. Stimulation of Fibroblast Proliferation The inflammatory response recruits fibroblasts to the site of injection.
Fibroblasts are key cells responsible for collagen synthesis. This process promotes:
o Neocollagenesis....
Editor's note: Dr. Weiss' extended-length letter can be read here.
03/03/2025
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Gary S Smit, DPM, Elliot Udell, DPM
I have seen this as a side-effect of medications. This is anecdotal, but I've seen it with anxiety medications like Zoloft and I saw it once as a side-effect from an artificial insulin product. This is very frustrating to treat. I think that oral antifungals is a good idea.
Gary S Smit, DPM, Kme, PA
I recommend doing the biopsy because if it turns out to be psoriasis or some other autoimmune disease, there are great new drugs available that can address these issues.
One patient of ours had psoriatic plaques all over his body. He went from dermatologist to dermatologist for years and still suffered. Finally, he was placed on Skyrizi and within a short period of time, he had resolution of all of his plaques and feels like a new person. Please let all of us know what the final diagnosis turns out to be.
Elliot Udell, DPM, Hicksville, NY
08/09/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Paul Kesselman, DPM
Kudos to Dr. Pressman for pointing something out which I have been preaching for my over 40+ years as a clinician. I first came aware of non-invasive vascular technology back in the late 1970s and early ‘80s during my undergraduate medical education at rotations at various VA hospitals in the Chicago area. In those days, the machines were big, bulky, and took up an entire room. Their costs and size relegated them mostly to large clinical or research facilities.
With computer technology, eventually the machinery got more sophisticated and totally paper free and can integrate directly into your computer and eventually into your patient's EMR. Most cost 1/3 of what digital x-rays cost, with many fitting into your briefcase. The current machinery can combine pulse volume recording and photoplethysmography, which are far more sophisticated than...
Editor's note: Dr. Kesselman's extended-length letter can be read here
05/01/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1B
RE: Functional Hallux Limitis
From: Howard Dananberg, DPM
Howard Bonenberger mentioned in a post last week that one of my lectures on functional hallux limitus (FHL) inspired him to treat patients with chronic postural complaints. I appreciate his comments and am glad he was able to find these concepts valuable. I have written extensively on FHL over my career, and have come to the realization that this concept remains misunderstood. The reason why it can impact postural form lies in the following principle. Once the hallux makes ground contact during any step, IT DOES NOT MOVE AGAIN UNTIL TOE-OFF. ln any form of hallux limitus (structural or functional), what is restricted is not the hallux, but the remainder of the foot and proximal structures all the way to the neck.
As the body adjusts for these motions, various sites are stressed repeatedly during each step cycle. And since these motions are repeated thousands of cycles per day, the stress becomes a chronic irritant. In particular, loss of MTP joint motion restricts heel lift, shortens stride length, and causes the ensuing swing phase to be altered in such a way as to make toe-off mechanically inefficient. Since the iliopsoas is the primary hip flexor at toe-off, and originates directly from the lumbar spine, it becomes the site of pain. The references for this are below.
Howard Dananberg, DPM
06/22/2023
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Elliot Udell, DPM
Glen, thank you for enlightening us on your successes with prolotherapy. Perhaps you can publish your technique as well as findings. If you can document that prolotherapy works, the treatment will no longer be in the realm of alternative healthcare. If the article is well written, there are many journals in our profession that would love to publish it. As for charges, I based this on what a certain non-podiatric physician in my geographic area was charging and it was well over a thousand dollars for each treatment. Some of these patients were quite upset after spending 10K, out-of-pocket, for a series of dextrose injections.
Elliot Udell, DPM, Hicksville, NY
05/24/2023
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: David Secord, DPM
A few years back, I wrote a book on pain management, but never found a publisher. There was a chapter on the use of potentiation so that you could obtain greater effect from a narcotic and use a lower dosage via use of a potentiator drug. There are different categories (tricyclics, anti-psychotics, anxiolytics, SSRIs), but they work the same way (the explanation of which is too long to cover here.)
Navane (Thiothixene), Xanax (alprazolam), and a few others have been used to varying effect. When I did an office procedure in my surgical room, I would have the patient take a Vicoprofen (hydrocodone and ibuprofen) [now discontinued] with a 5mg or 10mg Valium (diazepam) (dosage dependent upon body mass) with food about an hour pre-op. The majority of the patients slept through the procedure and the ones who were conscious appeared completely at ease and relaxed. The one med would potentiate the effect of the other without increased mu receptor activation and respiratory depression.
David Secord, DPM, McAllen, TX
05/04/2023
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Wenjay Sung, DPM, Todd Lamster, DPM
That’s cancer. Prove me wrong; get a biopsy or send out for a biopsy.
Wenjay Sung, DPM, Arcadia CA
Regarding the unidentified lesion on the dorsal aspect of the foot, this lesion needs to be biopsied as soon as possible to rule out carcinoma. With its rolled border, I would guess that it is a basal cell carcinoma.
Todd Lamster, DPM, Scottsdale, AZ
04/14/2023
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Edith James, CPed
Pedifix’s Pediplast made into a custom toe separator could be the solution. Custom toe separators can be made to lift and prevent rubbing between toes plus significantly reduce contact with ground forces. These are formed directly to the foot, then cure in minutes. These last very well; some last for more than a year.
These combined with cushioned, moisture-wicking high tech fiber socks have improved the health of many patients. Note: thicker socks usually require more room in footwear, of course. Personally, if current socks are inadequate protection, my presentation of solutions starts with socks since they’re the first opportunity to help. Custom toe separators, protective cushioned socks, orthoses, then fit footwear are all that are needed here.
Edith James, CPed, St. Louis, MO
01/09/2023
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Howard Dananberg, DPM, Lloyd Smith, DPM
I’ve had a great deal of experience both as an avid skier and podiatrist. My recommendation is to consider semi-weight-bearing impressions for custom ski orthotics. The foot is very compressed within the ski boot and full control can be quite painful. Lowering the MLA via the impression technique is very helpful. And since the medial column of the foot controls the medial edge of the ski, 1st ray cutouts permit improved 1st metatarsal plantarflexion, thereby improving edge control without the need for excessive posting or arch support.
Howard Dananberg, DPM, Stowe, VT
I skied about 60 days a year for over 20 years. I improved my technique and comfort by working on my old rohador orthotics using layers of duct tape on the medial edge to determine the proper pronatory control. After finding the sweet spot to gain symmetry and edge control, I took them back to the office and added Korex posts to match. They are met head length and I inserted a flat insole to fill out the shell. They eliminated all foot pain and allowed me to ski on any trail I wanted.
The foot should not move in a boot. That causes foot fatigue and poor technique. You should be skiing with your knees and hips with additional balance from your upper body and poles. I found it challenging to design ski orthotics for patients. Without an expert boot fitter, it is difficult. As a result, I developed a close relationship with the fitter and most patients were satisfied.
Lloyd Smith, DPM, Newton, MA
01/06/2023
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Lloyd Nesbitt, DPM
Orthotics for pronation in a ski boot would be very effective to improve ski edge control, lessen transverse plane motion at the knees, and reduce foot fatigue. (If the foot is pronated in the ski boot, then one has to use their knees more in order to set the inside edge of the ski when turning). While a “three-quarter length” orthotic from a shoe may work in a ski boot, often the interior of a ski boot heel area fits narrower than a shoe, and so there may be trouble fitting the orthotic to the back of the boot.
I suggest ordering a narrow grind to the orthotics with shallow heel cups and a vinyl cover with Poron or Lunasoft to the toes. Sending the lab a tracing of the ski boot insoles would be helpful— or better still, the insole itself. A rigid cavus foot type with an orthotic in a ski boot can be problematic because of the dorsal midtarsal area pressure from ski boot buckles — and most skiers with this foot type have to find a boot that will accommodate their foot type.
Lloyd Nesbitt, DPM, Toronto, Canada
01/05/2023
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Paul Betschart, DPM
I have been a skier for many years and have used custom and non-custom orthotics in my ski boots as well as have had them made for my patients. Since the feet are locked in the boot and there is no heel to toe motion, a thinner shell can be used. Extrinsic posting is rarely needed. Devices need to fit the contour of the bottom of the boot to sit properly. Send the original foot bed or at least a tracing to the lab with the prescription to get the correct shell width. Top cover choice is based on preference. Vinyl is the most durable and water resistant but many skiers want to "stick" to their boot for better control. A semi-rigid closed cell foam can be used in these situations.
Balancing for forefoot pathologies with relief pads, metatarsal pads, etc. can be helpful as proper skiing technique increases load on the forefoot. Patients with marked equinus may need a small heel lift to allow for proper forward lean. Don't ignore the boots themselves. Most ski boots have the ability to be adjusted in both forward lean and cant (varus/valgus). A good boot fitter should be able to make those adjustments as needed. I have used these principles to get orthotics to fit for other low volume footwear such as ice skates, racing flats, soccer cleats, etc.
Paul Betschart, DPM, Danbury, CT
11/18/2022
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Jengyu Lai, DPM, David Secord, DPM
I had the same question many years ago. I designed a multiplex PCR test with the idea of correlating the type of HPV and treatment efficacy. However, my research went to a different direction afterward. I'd be interested to see whether this assay could be used in the research.
Jengyu Lai, DPM, Rochester, MN
I don’t have any studies to quote on either the bleomycin or Panacos graft procedures for verrucae treatment. Observational studies are—like any form of empiricism—of little scientific value as “occurrence is not causation” and does not adhere to the guidelines of Koch’s postulates, the Bradford/Hill criteria or Falkow’s criteria. Anyway, I’ve treated flat warts with bleomycin and mosaic warts with the Panacos graft technique since 1999. Over several hundred bleomycin procedures, the cure rate has averaged 98%, with the added benefit that you only treat one lesion, and every wart the patient has (regardless of pedal or manual) are eliminated. I’ve rarely encountered mosaic warts, but of the 32 Panacos graft procedures I’ve done to treat these, they have all resolved. It would be nice to do a controlled trial of some sort, but as there is no money in it, I can’t imagine a grant or sponsoring agency. If these studies exist, I’d love to read them.
David Secord, DPM, McAllen, TX
10/06/2022
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Tom Silver, DPM, Martin M Pressman, DPM
The youngest patient I ever performed a permanent ingrown on was a 6 week old! The pediatrician sent him to me as the nail border was severely abscessed. It was either congenital or acquired, but either way, it is not too difficult to correct this permanently. I recommend having something sweet for the baby to suck on and numb with a 30 gauge needle. Be very quick and since the toe is very small, just take out a very small sliver. It helps to have a ring light with a magnifying lens when you do this too. I have performed ingrown procedures on many children and find that they are easier when they are infants and much more difficult as they become toddlers. Toddlers will fight and scream more and often will need some form of sedation such as Benadryl.
Tom Silver, DPM, Golden Valley, MN
I have years of experience with this issue and I can give you some hard won advice.
1. These are painful and need treatment. The baby does not “grow out of it.”
2. Do a P&A on both sides. This is a problem you do not want to revisit.
3. This can be done in the office; however, it is difficult to do with the baby kicking and crying and will wear both you and the staff out for the day. That said, I have done these in the office but I prefer to take them to the hospital and do them under anesthesia. I position them sideways across the table. I also block the toes with 1cc Marcaine for post-op analgesia.
4. You will need tiny Beaver blades, curettes, and P&A cotton tip applicators. Phenol sticks are too large but you can use the phenol with your own cotton tip applicators. You will need to supply the phenol packs.The hospitals never have the proper equipment and you need to bring in an office kit for them to re-sterilize a few days before the procedure.
5. Don’t be afraid to excise the hypertrophied nail fold at the same time. No sutures are required. I often use a tissue nipper for that. The youngest patient was about 3 months. I have seen younger, but would often do an office slant back until they were older and larger, and then bring them in for surgery.
Martin M Pressman, DPM, Milford , CT
08/18/2022
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Pete Harvey, DPM
I have used the one minute PA procedure for over 40 years and it works fine. I apply a snug Band-Aid and have the patient remove it the next day. I then have them apply isopropyl 70% alcohol bid x 2 weeks. Do not apply ointment, creams, etc. Showers are okay, but no baths or swimming are allowed until healing has occurred, which is about 4 weeks.
I apply phenol, then apply a dry pledget of cotton, then repeat one more time. I give the patient a post-op care sheet advising of a phenol flare at about 5 days and of drainage in about 3 weeks. I have the patient keep the toe open to the air as much as possible starting the second day post-op.
Pete Harvey, DPM, Wichita Falls, TX
04/21/2022
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: John Lanthier, DPM
In response to Dr. Kass' inquiry, I have heard of practitioners utilizing this injection mixture although I have never done this. When questioned as to the reason why they did it, the response was that they didn't believe that ETOH was an effective treatment and also didn't believe in the protocol so they used cortisone in with the ETOH to achieve a clinical result.
In the picture shown, I don't believe that the mixture of the two medications caused that tissue destruction but more than likely a high dose of injectable Marcaine with a high dose of epinephrine combined with a high percentage of ETOH placed too superficially and also into the intermetatarsal artery. The three combined caused vascular collapse and necrosis. Just a theory. It gave me concern seeing the result. I feel for the doctor and the patient.
John Lanthier, DPM, Sudbury Ontario, Canada
04/18/2022
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Andrew Cassidy DPM, MS
The spike protein in Covid virus definitely has micro clotting issues as do the vaccines. That is why you no longer can get the J&J shot (however they all have this issue). Make sure to ask if the patient was vaccinated for Covid. I have seen several odd vascular and neurological manifestations from the initial infection and vaccine. Check for elevated D Dimer, CRP, and Sed rate.
I had a patient with similar non-healing wound post-vaccine and I put him on 10mg prednisone and 325mg aspirin and the wound turned around and quickly healed. Often we are told not to use steroids for wound healing, but in a case like this it may be the correct choice. I also think good vitamin supplementation with vitamin D,C, and with zinc are all good for healing as well. Don’t be afraid to think outside of the box on Covid. The medical profession has not done its due diligence during the past 2 years and failed to apply critical thought.
Andrew Cassidy DPM, MS, Austin, TX
04/15/2022
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Richard Foster, DPM
Take a biopsy and culture for an acid fast stain which might identify a mycobacterium species not found in other standard staining techniques. I have seen this in a swimming pool injury that would not heal in a child. The child had mycobacterium marinum, also seen commonly from a fish tank inoculation. Mycobacterium comes from water, soil, and dust. Getting stepped on from a high heel could be like an inoculation. I think you need to rule this one out before categorizing it a COVID-19 possibility.
Richard Foster, DPM, Hackensack, NJ
07/14/2021
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Dennis Shavelson, DPM, CPed
I have taken the liberty to edit and re-post the x-rays to demonstrate that this case has been under-appreciated in its biomechanical scope.
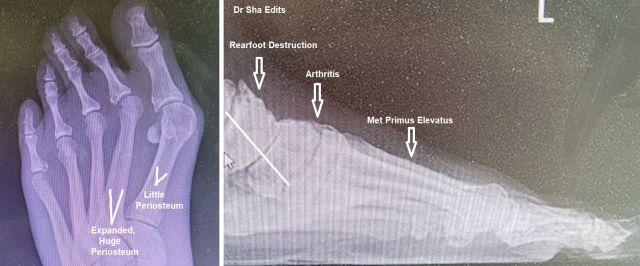 |
Pre-op weight-bearing x-rays |
• This seems to be a late stage rigid rearfoot-flexible forefoot foot type with a medial column met adductus, suggesting an injury or overuse.
• The rearfoot-midfoot shows advanced under-vaulted biomechanics and arthritis.
• The 1st ray is holding very little closed-chain weight for years; witness the thin periosteum and demineralization.
• Dramatic excess weight exists under the 2nd met head for years; witness the huge expansion of the bone itself horizontally + the massive periosteum. Also note the almost absent medullary canal which is reducing shock absorbency.
• Biomechanical questions: Patient’s other foot presentation? Is there an LLD? Ankles, knees, hips, pelvis, and lower back biomechanics? Patient's activity level? Any neuromuscular imbalances? Patient’s expectations beyond relief of her 2nd Met head pain?
I suggest adding rocker shoe insoles to all footgear and a custom functional foot type specific foot orthotic plus specific lifestyle modifications and health coaching. Surgically, consider the heroic procedure of a 2nd met head hemi-resection osteotomy or a 2nd met head resection as an isolated procedure.
Dennis Shavelson, DPM, CPed, Tampa, FL
07/13/2021
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: David E. Samuel, DPM
This looks very similar to a procedure we did just a few weeks ago. She had a bumpectomy as a young adult which clearly was useless. She developed this over 30 years, with similar complaint of pain to the forefoot and she was unable to wear shoes. We did not feel an added head osteotomy was the play as she already had post-surgical changes from prior surgery and long-standing remodeling and the joint was not painful, so an Akin worked here for us. Lately, especially with Lapiplasty, I do the Akin more. l then try to make the foot look perfect with a corrected first met head, using a Reverdin-Green type osteotomy, etc., as the goal is comfort and fitting into shoes.
The lateral view did not show any first ray elevation, but a Lapiplasty is quite good in allowing some first ray plantarflextion if necessary. Here is what we did. Met adductus mets 2 and 3, Weils to help with length and digital lateral deviation, Lapiplasy, distal Akin, and arthroplasties as necessary. PWB (Impossible to be NWB due to her size and general conditioning, but in general, only few things I keep full NWB, and with Lapiplasty, of course. WB immediately post-op is such an awesome perk of the procedure. This for those who are yelling “what!, weight-bearing ?”), CAM boot. She is doing quite well. She is now about 6 weeks post-op. Osteotomies all showing healing.
David E. Samuel, DPM, Springfield, PA
04/19/2021
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Robert S. Schwartz, CPed
Overuse, repetitive stress injuries from excessive forces occur during the propulsive phase of gait, particularly in the sagittal plane. Managing motion is an effective way to relieve these forces.
 |
High-toe-box, extra-depth, athletic walking shoe with built-in (L) and added rocker (R). |
These photos reflect the use of high-toe-box, extra-depth, athletic walking shoes with built-in rockers. When increased motion control is needed, an additional rocker is added to increase toe-spring (dorsiflexion motion mitigation).
Disclosure: I have no fiduciary relationship with Apex.
Robert S. Schwartz, CPed, NY, NY
04/06/2021
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Don Peacock, DPM
I agree with Dr. Katzen on the idea of performing a 3rd metatarsal osteotomy for some cases. In my traditional training, I would have disagreed with him. However, having learned MIS, I know the procedure is valuable. It needs more studies and scientific backing although literature exists for the technique.
A helpful technique for me is to not only look at metatarsal parabola but also use diagnostic ultrasound. If you look at the forefoot and determine swelling/edema in the 3rd MPJ, the anatomy confirms the issue is in the 3rd met and an osteotomy could be performed or maybe something even better.
Metatarsal osteotomies only work with...
Editor's note: Dr. Peacock's extended-length letter can be read here.
03/17/2021
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Dennis Shavelson, DPM
Dr. Dananberg and I have spent years proclaiming that the forefoot medial column and peroneus longus are the primary keys to functional lower extremity biomechanics and not the subtalar joint or rearfoot pronation. The problem has four components: a structural defect in the forefoot, a myofascial component allowing soft tissue flexibility, a peroneus muscle engine atrophy of disuse, and a neural strategy that has lost motor control of PL.
This requires structural optimization, muscle engine training, myofascial restoration, and neural strategy rebooting. Custom or customized corrective foot orthotics, stabilizing and compressing, kinesiology taping, foot centering pads, and compensatory foot centering training are all required.
All else including isolated foot orthotics, training, and surgical procedures are Band-aids or will biomechanically create new and possibly worse biomechanical sequelae in the feet and elsewhere over time.
Dennis Shavelson, DPM, NY, NY
03/09/2021
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Allen Jacobs, DPM
The first principle of medical ethics is that of patient autonomy. Given truthful and accurate presentation of facts without bias or coercion; a patient has the absolute and ultimate right to self-determine what diagnostic and therapeutic efforts will be pursued. The risks of “no treatment” should be discussed (and documented as understood).
As a healthcare provider, you are not obligated to administer care which you do not feel is in the best interest or even harmful for a patient. You do have an obligation to assure proper transfer of such patients for care elsewhere. As for the “lawyers having a field day”, I am not a lawyer; however, I suspect the realities are not so simplistic. The days of paternalistic medicine mandating unquestioned care are no more.
You are likely best-served not treating patients with whom you are not comfortable. You indeed have that option. However, to suggest that all such patients should be summarily discharged for fear of litigation and liability may be overly simplistic. Decision-making is a mutual effort between patient and doctor.
Allen Jacobs, DPM, St. Louis, MO
02/22/2021
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Howard Dananberg, DPM, Paul Jones, DPM
Here is a treatment I’ve used successfully for many years... 200mg of coenzyme Q10 given QD. It works in just several days and is very safe.
Howard Dananberg, DPM, Stowe, VT
I've mentioned before that Raynaud's phenomenon/chilblains often responds well to L-methyl folate. It doesn't interact with any medications. It is commonly used for depression, diabetic neuropathy, Alzheimer's disease, and even as a prenatal vitamin. The only thing recommended is to take with B12 to avoid anemia. It often comes mixed with the B12 to simplify this process. It may be contraindicated with cancer or a history of seizures. If this is the case, have them clear with their PCP prior to starting. In less severe cases, I have them use it seasonally. It can be used in the pediatric through geriatric patient.
There is no problem having the patient start or stop on a dime. Sometimes there can be some temporary insomnia for the first two weeks when first starting the medication. So have them take qd in the AM for a couple of weeks. The patient usually needs to use at least 3 months to decide if it will work for them. It is easier to use without side- effects than Minipress or Nitro paste, and possibly even cheaper. As Allen Jacobs, DPM has mentioned before, a good source of this product is through EBM medical.
Paul Jones, DPM, Happy Valley, OR
|
| |

|
|
|







