





|

|
|
|

|
Search
05/13/2014
RESPONSES/COMMENTS (CLINICAL)
From: Bryan C. Markinson, DPM
There are several topical treatments for both basal and squamous cell carcinoma, PROVIDED that the lesions are singular and have not spread to lymph nodes. The poster does not say why the patient is homebound. In any case, before treatment is begun, the patient needs a total body survey and lymph node exam. In my opinion, topical treatment of these cancers is best left to those who do it regularly, or if in this situation, it is possible for the DPM to consult with a dermatologist for advice, I would do so. I would definitely not fly solo, especially since the full evaluation of this may raise scope issues for the DPM. Kudos for the clinician who did the biopsy to get the diagnosis.
Other messages in this thread:
08/20/2025
RESPONSES/COMMENTS (CLINICAL)
From: Gary Unsdorfer, DPM, Lawrence Kassan, DPM
After reading the post regarding the post-operative infection of a repaired Achilles tendon, two points come to mind.
1. If the graft and Achilles tendon repair was decimated during debridement of the post-op infection, would not this lead to a dorsiflexed position of the foot rather than equinus?
2. I find it extremely hard to believe that the patient could be walking 7 miles per day at only 4 months post-operatively following any type of Achilles repair, especially given the history of R.A.
Gary Unsdorfer, DPM (retired), Medina, OH
I had a very similar patient after removal of a large retrocalcaneal spur and Speed bridge reattachment. There was about a 1.0 cm distal portion of her incision that probed fairly deep and did not respond to conservative wound care. I admitted her and placed her on IV Vanco, took her to the OR for a debridement, antibiotic pulse lavage, and packed the wound with an Orthobiologic graft and closed the wound primarily. She healed without incident.
Lawrence Kassan, DPM, Philadelphia, PA
08/19/2025
RESPONSES/COMMENTS (CLINICAL)
From: Mark Spier, DPM
If your ID consultant hasn't done so yet, try to obtain a fungal culture from the wound. S. hominis may not be the causative organism responsible for this wound infection. Sometimes a mycological etiology cannot be definitively identified, so empirical antifungal therapy may provide a resolution in this instant case as it did for a similar patient of mine many years ago. Best of luck!
Mark Spier, DPM, Reisterstown, MD
08/07/2025
RESPONSES/COMMENTS (CLINICAL)
From: Robert Scott Steinberg, DPM
About seven years ago, I received a series of 5 Synvisc injections in my knee. My knee pain was reduced by 80%. This allowed me to ski. The following year, I received Synvisc One. It reduced my pain by 99%. I then received Synvisc One twice a year for three more years, until it no longer helped. I went on to have a Stryker Triathlon knee replacement, eliminating 100% of the pain.
Perhaps Synvisc One would work better in the ankle.
Robert Scott Steinberg, DPM, Schaumburg, IL
06/13/2025
RESPONSES/COMMENTS (CLINICAL)
From: James Hatfield, DPM
I have about 40 years experience with hyaluronidase injections for scar tissue. It's an invaluable tool. I generally create a "cocktail" with haluronidase, triancinalone acetate, Decardon, and Marcaine: 1/4cc, 1/4cc, 1/4cc,1/2cc, respectively. It's not comfortable to give the injection without giving a local anesthetic block proximally. I advise they could experience a post-injection flare from the steroids. I have had universal success with this injection, but sometimes less than 100% relief. Still, every patient has been happy they had the injection. I have never had an adverse response.
James Hatfield, DPM, Encinitas, CA
06/05/2025
RESPONSES/COMMENTS (CLINICAL)
From: Bradley J. Makimaa, DPM, Vince Marino, DPM
Please excuse me if I am missing the point. However, I have spent 27 years shortening symptomatic toes. I believe that lengthening the third and fourth toes is doomed to failure and should not be done. Rather, wait until the bunion and hammertoes are symptomatic and do a bunion procedure with shortening, a second arthrodesis with shortening, and a fifth toe arthroplasty, and then you will have a uniform foot. Don't treat the x-ray.
Bradley J. Makimaa, DPM, Key West, FL
Perhaps it is because Drs. Gurnick, Roth, and I are old and have been in practice for too many years, but I echo their sentiments. Keep it SIMPLE. First, if it is a functional problem, then just do arthroplasties of the toes and possibly a cylindrical Akin of the hallux. But if for cosmetic reasons, I highly suggest you send the patient elsewhere as this patient will never be happy with anything you do; and do you really need the future headaches for the little amount you will be reimbursed.
Vince Marino, DPM, Novato, CA
06/04/2025
RESPONSES/COMMENTS (CLINICAL)
From: Keith L. Gurnick, DPM, Ivar E. Roth, DPM, MPH
There surely might be other considerations, and we do not know if this is for functional issues or purely cosmetic concerns, and not limited to the size, length, and appearance of the RIGHT foot. Why not offer the patient the idea to simply shorten the hallux and the 2nd toe at one surgical setting?
Keith L. Gurnick, DPM, Los Angeles, CA
Rather than make this complex, just do arthroplasties of the 2nd and 5th toes and make them all the same length. It’s much better and easier with less complications and the patient will be happy.
Ivar E. Roth, DPM, MPH, Newport Beach, CA
05/19/2025
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: David Secord, DPM
Some years back, I was treating a border patrol agent who caught a Mesquite tree thorn in her thumb. She was “treated” at the E.R. and was still having problems. Why? Upon examination, the thumb was about twice the expected diameter—indicating that a foreign body was still present—and the incision made was closed with 2.0 Ethibond. In this case, an examination of the procedure revealed that this was not done by a doctor, nor a PA. Not done by a NP either. This atrocity was committed by an MA. They had a medical assistant (who, rather obviously has zero qualifications or permission to perform a surgical procedure on anyone) inject, incise, poke around, not find, and suture with totally inappropriate material a foreign body procedure.
I don’t know if this relates to the hernia procedure, but one never knows. I recently inherited a patient post-hallux amputation procedure who was told (and given written instructions) that he could immediately start bathing the site, still sporting the nylon sutures. I don’t know if I’ve missed something new, but the “go ahead and bathe immediately post-op” idea isn’t supported by any science and is strongly opposed as far as I’m aware. There is some questionable stuff out there.
David Secord, DPM, McAllen, TX
05/16/2025
RESPONSES/COMMENTS (CLINICAL)
From: Ron Werter, DPM
What a surprise! A permanent procedure works better than a non-permanent procedure for preventing re-occurrence of a problem. They weren’t talking about a Frost or Winograd, just a regular CPT 11730. Are you sure this wasn't dated April 1.
Ron Werter DPM, NY, NY
04/24/2025
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: David T. Weiss, DPM
The effective concentration of dextrose is 50% (hyperosmolar).
Mechanism of Action of Dextrose:
1. Localized Inflammatory Response Dextrose solutions (typically hyperosmolar) act as an osmotic irritant when injected into entheses, ligaments, tendons, or joint capsules. This mild irritation triggers a controlled, localized inflammatory response.
2. Stimulation of Fibroblast Proliferation The inflammatory response recruits fibroblasts to the site of injection.
Fibroblasts are key cells responsible for collagen synthesis. This process promotes:
o Neocollagenesis....
Editor's note: Dr. Weiss' extended-length letter can be read here.
04/24/2025
RESPONSES/COMMENTS (CLINICAL) - PART 1A
From: Ron Werter, DPM
My suggestion is to take a course and get certified. Don’t screw around with it. The least you can do is be ineffectual, the worst is to cause damage.
A close friend of mine is an MD whose practice is exclusively prolotherapy. After 20 years doing this, he is still taking additional courses. I asked him about my doing this in my practice for heel pain. "Sure," he said, "but take the course. It’s not as simple as you think."
Ron Werter, DPM, NY, NY
04/10/2025
RESPONSES/COMMENTS (CLINICAL)
From: Richard M. Maleski, DPM, RPh
I also had a case almost identical to this one in question. I originally saw the patient when she was 5 years old, complaining of multiple painful "shiny things" on multiple toes. She had the reddish brown papules in the symptomatic areas. Nothing was found clinically or on x-ray. She presented again as a young adult many years later with the same complaint. She stated that she found black filaments in the areas when she looked for them. Once again, I could find nothing on examination. I had a difficult time doing a neuro exam, since she complained of severe pain with manual muscle testing and with percussion of the superficial nerves looking for a Tinel's sign.
Consultations and workups with a neurologist and rheumatologist yielded no results. Her PCP placed her on gabapentin. About a year later, she developed severe CRPS secondary to an ankle sprain, despite my immediately sending her to physical medicine and aggressive physical therapy. Another year or two after that, she developed severe CRPS of her upper extremity, after a bruising injury to her hand. She had been treated by a psychiatrist for many of those years also, but, unfortunately, none of the treatments by any of the other physicians seemed to have any effect. She passed away at a relatively young age due to heart failure. Neither myself nor any of the other doctors were able to make a definitive diagnosis.
Richard M. Maleski, DPM, RPh, Pittsburgh, PA
04/09/2025
RESPONSES/COMMENTS (CLINICAL)
From: Bruce Kaczander, DPM,
It is highly unlikely that it’s a bilateral symmetric foreign body and highly unlikely that a 1 mm macule would cause pain like that. If she is having symptoms at bedtime (HS), consider something neurogenic. Tarsal tunnel will cause HS symptoms due to engorgement of venae comitantes. Do a Tinel’s test.
Radiculopathies can cause HS pain, even in the absence of current back pain. Is there a history of spinal issues? Bottom line, start her on gabapentin or Lyrica and titrate the dose as needed.
Bruce Kaczander, DPM, Livonia, MI
04/08/2025
RESPONSES/COMMENTS (CLINICAL)
RE: Invisible Metallic Fragments (Morgellons Disease?)
From: Joel Feder, DPM, Name Withheld
My experience with Morgellons disease was with some heavy recreational drug users. Get an extensive history.
Joel Feder, DPM (Retired), Sarasota, FL
I had a similar case involving a massage therapist who presented with lateral heel pain. He reported stepping on a fishing hook three months prior while fishing but couldn’t recall whether the hook had broken off. Since then, he had been experiencing persistent pain. Interestingly, when he placed a magnet on the heel, it stuck. Initial imaging, including x-ray and ultrasound, revealed nothing abnormal. Two months later, he returned—this time with pain in the opposite foot. He admitted he might have been mistaken about which foot had stepped on the hook. Once again, the magnet adhered to his heel, but imaging was inconclusive.
During this second visit, I conducted a more thorough physical examination and was able to reproduce the pain. I diagnosed him with bursitis, and he was satisfied with the explanation. In hindsight, I regret relying too heavily on his knowledge of soft tissue anatomy due to his profession. Yet, I still find myself puzzled—how did the magnet stick to his heels?
Name Withheld
03/04/2025
RESPONSES/COMMENTS (CLINICAL)
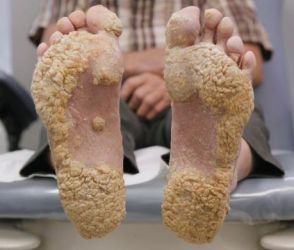
RE: Plaque-Like Calluses on Weight-Bearing Surfaces
From: PM News Subscriber
This is a picture after I scraped away most of the plaque-like calluses. From this, I used a skin curette and obtained keratin samples that were sent to the lab for PCR testing. Results in three days. The lab returned: MRSA. I would do this before any invasive biopsy.
 |
Plaque-Like Calluses on Weight-Bearing Surfaces |
It treated well with mupiricin 2% ointment for one month.
PM News Subscriber
03/03/2025
RESPONSES/COMMENTS (CLINICAL) - PART 1B
From: Gary S Smit, DPM, Elliot Udell, DPM
I have seen this as a side-effect of medications. This is anecdotal, but I've seen it with anxiety medications like Zoloft and I saw it once as a side-effect from an artificial insulin product. This is very frustrating to treat. I think that oral antifungals is a good idea.
Gary S Smit, DPM, Kme, PA
I recommend doing the biopsy because if it turns out to be psoriasis or some other autoimmune disease, there are great new drugs available that can address these issues.
One patient of ours had psoriatic plaques all over his body. He went from dermatologist to dermatologist for years and still suffered. Finally, he was placed on Skyrizi and within a short period of time, he had resolution of all of his plaques and feels like a new person. Please let all of us know what the final diagnosis turns out to be.
Elliot Udell, DPM, Hicksville, NY
03/03/2025
RESPONSES/COMMENTS (CLINICAL) - PART 1A
From: PM News Subscriber, David P. Luongo, DPM
This is a picture of my patient with T-cell lymphoma. A biopsy of your patient may be a good idea.
 |
Plaque-Like Calluses on Weight-Bearing Surfaces |
PM News Subscriber
I've seen this before. For my patient, it was the onset of menopause where there was a sudden change in hormones. Have that checked out.
David P. Luongo, DPM, Paramus, NJ
02/04/2025
RESPONSES/COMMENTS (CLINICAL)
From: Chuck Langman, DPM
I am also in the Philadelphia area and refer to David Dwyer, MD at Jefferson University Hospital. I believe he does pinpoint radiation for it. I’m not sure if that is appropriate for an 11-year-old but it is certainly worth the call.
Chuck Langman, DPM, King of Prussia, PA
12/12/2024
RESPONSES/COMMENTS (CLINICAL)
RE: Can a Nail Like This Ever Regrow Normally?
From: Christopher Stewart, DPM
The short answer is “YES”, a gryphotic/mycotic nail CAN grow back normally if the root causes are properly addressed. Over the past 20 years, I’ve had more successes than failures in tackling these nails. In my experience, osteochondromas are only a small part of the overall solution. We find these growths need to be removed about 74% of the time.
 |
Before and after photos |
As an aside, I no longer perform radiographic screening for these deformities because intraoperatively I was often getting surprised by chondromas once the offending nails were avulsed. These firm, protruding radiolucent chondromas must also be removed because they are just as problematic to nail attachment as true “bone spurs”.
Christopher Stewart, DPM, Charlottesville, VA
12/11/2024
RESPONSES/COMMENTS (CLINICAL) - PART 2
From: Ron Har-Zvi, DPM
The onychomycotic hallux nail can grow back normally if it is caused by an underlying subungual exostosis, either osseous or cartilaginous. I am retired but when I was practicing, I was 3 for 3 on correcting this condition. All 3 patients were in their 40s or 50s, and all 3 nails were normal after 1-2 years. The mycotic nail was removed 2-3 weeks before the bone surgery.
Ron Har-Zvi, DPM, Wayne, NJ
12/11/2024
RESPONSES/COMMENTS (CLINICAL) - PART 1
From: Ivar E. Roth DPM, MPH, Jeffrey Kass, DPM
It is possible but first you must get rid of the fungus. Sometimes you may have to use ½” paper tape at the distal end of the toe to hold down the soft tissue. I am trying something new and that is applying a KeryFlex nail to put pressure on the distal tip to flatten out as the nail grows over. I will report on if this works. Plan on treating for an extended period of time as these nails are difficult to convert to “new nails”, but I have done it on occasion.
Ivar E. Roth DPM, MPH, Newport Beach, CA
I thank Dr. Weiss for linking us to his informative and very well written article on onychocrptosis and subungual exostosis. I am not sure how often the abnormal nail is a result of abnormal distal phalanx, but the intimate relationship he brings up is certainly of clinical value. Good job.
Jeffrey Kass, DPM, Forest Hills, NY
12/10/2024
RESPONSES/COMMENTS (CLINICAL)
From: David T Weiss, DPM, R. Alex Dellinger, DPM
Regarding the above question, it is common for a nail to grow poorly due to the underlying bone. Remember, the nail grows right on top of the distal phalanx. If there is an underlying bony or cartilage defect, the growth of the nail will continue to be pathological. Once the defect is surgically removed, the nail matrix typically creates more cosmetically pleasing nail tissue.
It takes SEVERAL nail cycles for this to happen, and the patient needs to be educated that it will take a while before they notice improvement. In addition, I will have my patients take collagen powder and Biotin. I published a recent paper on this condition and the treatment options involved in managing the growth of the nail.
David T Weiss, DPM, Richmond, VA
No.
R. Alex Dellinger, DPM, Little Rock, AR
12/06/2024
RESPONSES/COMMENTS (CLINICAL)
RE: Treatment of Onychomycotic Onycholysis
From: Elliot Udell, DPM
The toenail depicted is something we see commonly. It may be caused by trauma to the matrix and/or the underlying bone. Severe onychomycosis which damaged the root of the nail may be a culprit, or it may be an arthritic spur on the bone which is pushing up and not allowing the nail to grow out. Because the patient was living with this for a long time, conditions beneath the underlying nail present a perfect medium for all sorts of fungi and bacterial growth.
Culturing that area is akin to culturing the bottom of a garbage can. You will see lots of things growing which may not be clinically relevant. Treatment options: Debride the non-attached nail back to where it is still attached or remove the entire nail and give the patient a slim hope that it will regrow normally. Removal of the matrix is also a possibility and then the "sick" nail will be history. X-rays of the toe should also be taken to rule out a dorsal exostosis, and if this exists, it may have to be addressed surgically. If you do, opt to remove the entire nail with or without a matrixectomy; the specimen should be sent to a dermatopathology lab where they will examine the attached skin and make sure that you are not dealing with a neoplastic disease.
Elliot Udell, DPM, Hicksville, NY
10/15/2024
RESPONSES/COMMENTS (CLINICAL)
From: Kenneth Meisler, DPM
If you write enough Jublia, you are going to see the1-2% adverse reactions including dermatitis, vesicles, and pain that were described in the clinical trials. They did not describe it as an allergic reaction. If you write enough Jublia, you will see these reactions and I have. Dr. Lanthier thought it looks like the sequela from an onychia. I do not agree. I have found that it always responds to treatment as if it were an allergic reaction. I instruct the patient to discontinue the medication and apply topical steroid cream. If it were an onychia, some of the patients would probably not respond to that treatment.
Dr. Blum said, "one of the warnings when using Jublia is to avoid using on the skin." The application instructions state to apply to the nail and the "folds of the skin next to the sides of the toenail and underneath the end of the toenail," which is what I tell all patients. Interestingly, I have had patients who were on Jublia for many months before they started to develop these allergic-like symptoms, and many of them were extremely disappointed they had to stop because they were already seeing improvement. The very small amount of easily treated adverse reactions make Jublia an extremely safe medication.
Kenneth Meisler, DPM, NY, NY
10/14/2024
RESPONSES/COMMENTS (CLINICAL)
From: Larry Price, DPM
I actually saw an identical case/reaction to Jublia this week on all 10 toes. Immediate cessation and application of topical steroid cleared it up in a week.
Larry Price, DPM, Westwood, NJ.
10/12/2024
RESPONSES/COMMENTS (CLINICAL)
From: John Lanthier, DPM, Donald Blum, DPM, JD
There is a 1% incidence of onychia and 1% incidence of onychocryptosis from the use of efinaconazole according to the safety information packet. This looks like the sequela from an onychia.
John Lanthier, DPM, Sudbury, Ontario
One of the warnings when using Jublia is to avoid using on the skin. Perhaps the patient had a reaction to the medication getting on the skin? See the medication insert and warnings.
Donald Blum, DPM, JD, Dallas, TX
|
| |

|
|
|







