Dr. Graziano: Can you please describe the flap that you used in this interesting case of tophaceous gout?
John D Lanthier, DPM, Sudbury, ON
06/02/2017
QUERIES (CLINICAL) - PART 1
Query: Curled Nails in 8 Year Old Boy
This is a healthy 8 year old boy. Developmentally, he was a little delayed with walking - 14 months. He seems to be a fairly habitual toe-walker. His parents try to encourage correct walking, purchase shoes with stiffer soles, yet it still persists. There is certainly a considerable amount of forefoot ambulation with virtually no heel-toe. Periodically, there is slight in-toe left. He does not trip or fall. He has a deviated-curled varus 2nd toe at the DIPJ bilaterally.
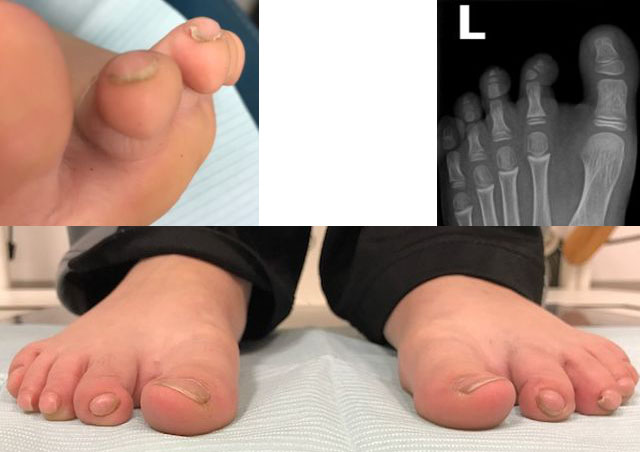 |
Curled Nails in 8 Year Old Boy |
The main concern is the ends of his toes and nails. He is doing Karate, with pain to the distal toes and nails. Cutting his nails has always been a chore for mom. Sometimes, bleeding occurs. The nail beds appear to be rounded with a slight dorsal bump with the nail curling over. The DIPJ is in rectus, with no 'fixed' or rigid contracture. Any advice would be appreciated.
07/18/2016
QUERIES (CLINICAL) - PART 1A
From: Sam Bell, Simon Young, DPM
I have found that toes that look like that always have responded to Diflucan.
Sam Bell, DPM, Schenectady, NY
Block the toe, remove the fibular 1/3 of the nail, excise the granuloma, and apply AgNO3. If need be, send the nail, matrix, and pyogenic tissue to a path lab. Long-term antibiotics don't work. Get rid of the mechanical cause.
Simon Young, DPM, NY, NY
06/11/2015
QUERIES (CLINICAL) - PART 1A
From: Jeff Kittay, DPM
While a pan met head seems the more radical procedure, in the long run, you will best serve this patient by doing what is needed. More limited procedures now only make it likely that you will need to do more later. If she is healing ulcers with A-1Cs in the 8s, then she is quite likely to heal the pan met procedure, assuming careful dissection by you. By all means, speak with her PCP/diabetologist regarding control of her sugars, but you'll have a happier patient sooner, with one surgery, than you will several years down the road with multiples.
Jeff Kittay, DPM, Boston, MA, Boston, MA
11/28/2009
RESPONSES / QUERIES (CLINICAL) - PART 2
RE: Osteomyelitis (Richard Frost, DPM)
From: Multiple Respondents
Dr. Richard Frost has a 64 year old patient with diabetic neuropathy of the 3rd and 4th proximal phalangeal bases and likely also their associated metatarsal heads. This was caused by extruding nail from footgear. There is no way to be able to "promise" a neuropathic diabetic patient any result from any form of treatment or non-treatment.
This case cries out for multiple consultation, and the consideration of an extended period of non-weight-bearing and IV antibiotics, with close monitoring for extension of the infection, prior to surgery. This patient will have to accept the "unlucky" aspects of his disease and not shunt them over to his physicians. This is a situation where a "heart to heart" talk with the patient and his family are not only recommended, but absolutely necessary. This condition is not the "fault" of his doctors, and the patient's attitude sounds like the ground-zero building of a lawsuit.
Michael M. Rosenblatt, DPM, San Jose, CA, Rosey1@prodigy.net
Dr. Frost may treat osteo with six weeks of antibiotics as opposed to surgery. He may want to open and culture but most likely will get a negative culture. I think an MRI as being diagnostic for osteo is way overrated. I have seen many false positives treated with unnecessary operations, and even amputations on people with Charcot joint, RA, and chronic gout. In my opinion, if there is no direct positive cause (like an ulcer to the bone), you should perform T99 and indium (or a similar) bone scans to diagnose osteo. Remember, if the indium scan is not more intense than the T99 scan, it is not diagnostic for osteo. The only 100% diagnosis is made by excision and culture.
Gary S Smith, DPM, Bradford, PA, penndoc@verizon.net
I can't tell what type of patient this is or what type of doctor-patient relationship you have with this gentleman. I don't think there is enough information to give a great answer as to the best procedure. If, however, this is a patient who does not show an understanding or respect for the position you are both in as a patient and surgeon, then the best procedure may not be one at all. This is a patient to whom I would state, in writing and orally, that in all likelihood, there will be another surgery in the future.
Jonathan B. Purdy, DPM, New Iberia, LA, podiatrist@mindspring.com
10/03/2009
QUERIES (CLINICAL)
Query: Subtalar Joint Implants Backing Out?
Has anyone experienced trouble with subtalar joint implants backing out? If so, what do you think was the cause? What did you change that helped address the problem?
Juliet Burk, DPM, Muskogee, OK
06/11/2009
QUERIES (CLINICAL)
Query: Best Procedure for Shortening Toes
I have a patient (40's) in good health who wants her 2nd and 3rd toes shortened. What is the best procedure for this? Is the middle phalanx removed and then the toe pinned for alignment? Also, is it a covered insurance procedure or is it always considered cosmetic?
Robert S. Adelman, DPM, New York, NY
06/06/2009
QUERIES (CLINICAL)
Query: Sandal Suggestions for an Elderly Patient with Flatfeet.
I have an elderly woman who has been looking for a pair of sandals-- not the "thong" style -- for her flat feet. She does not desire a custom pair. If they would be able to accommodate her current orthotics-- even better! I am looking for any reasonable suggestions.
Hans Blaakman, DPM, Duncan, SC
06/05/2009
QUERIES (CLINICAL)
Query: Spontaneous Blisters
I have a 65 year old female who presented with spontaneous blisters. She relates mild pain from these areas. They presented on the left hallux and right 2nd and 4th toes, however, have shown up on other toes in the past. They resolve after a while, but the patient is concerned as to why they continue to arise.
.jpg) |
Spontaneous Blisters |
She relates no past medical history but some sensitivity to cosmetics. No allergies otherwise and no significant medical history. Any suggestions or thoughts?
Jeffrey E. Kleiman, DPM, Fort Myers, FL
06/04/2009
QUERIES (CLINICAL)
Query: Calcific Mass of The Plantar Heel
I would appreciate any recommendations regarding treatment options for this 65 y/o diabetic female with a slowly enlarging mass of the plantar medial heel over the past 7 months. The mass has enlarged to the point where it has become painful with ambulation. There is a visible protuberance at the plantar medial heel and the mass is firm with palpation and only tender with deep palpation. There is no history of trauma, but she does admit a history of "heel spur injection" to this foot by her PCP at least several years earlier. She is a well-controlled diabetic with good vascular status and appears to be a good surgical candidate if it should come to that.
 |
Calcific Mass of The Plantar Heel |
MRI report as follows: "a probably benign extensively calcified mass medially in the plantar part of the foot near the calcaneus that measures 3.0 x 2.3 x 2.8 cm. Most of the mass is calcified. There is a soft tissue component that does enhance mildly. The etiology of it is not certain. The adjacent plantar fascia appears to be normal so it does not appear to be related to plantar fibromatosis."
Would needle biopsy be recommended prior to total excision? Partial vs total excision? If total excision is indicated, are there any recommendations regarding the soft tissue defect that would result following excision of such a large mass?
James Anderson, DPM, Lewisburg, PA
06/03/2009
QUERIES (CLINICAL)
RE: Terminating a Podiatry License
I have a license in a state that I will never practice in and never have, and it is up for renewal. I want to know what advice can be given regarding a license in a state that a podiatrist has never practiced in. Is it any different than a state that a physician does practice in? Is there a "right" way to give up the license? Any input would be greatly appreciated.
Philip E. Larkins, DPM, Escondido, CA
Editor’s comment: PM News does not provide legal advice. You should inquire with the licensing agency as to the state’s policy. In many states, you can change your license to “inactive” or “retired” status. In other instances, you simply inform the state that you do not intend to renew your license.
05/28/2009
QUERIES (CLINICAL)
Query: Interosseous Lipoma
I have a patient, 33 yo approx. 320 lbs. who has an intraosseous lipoma occupying about one third of the anterior aspect of her calcaneus. She wants it removed. I plan to pack the deficit with allograft bone chips. Any other suggestions, such as BMP or matrix materials?
Mike Werner, DPM, Largo, FL
05/27/2009
QUERIES (CLINICAL)
Query: Hand-Foot Disease From Chemo
Does anyone have any experience with Hand-Foot disease caused by chemo drugs? This is not the hand-foot-mouth disease found in children. The only thing I know about treatment for this condition is to avoid heat. Any other ideas?
Karen Malley Banks, DPM, Thomasville, GA
05/26/2009
QUERIES (CLINICAL)
Query: Abnormal Toenails in 3 y/o Boy
A 3 y/o otherwise healthy boy was recently sent to me by his pediatrician. He has very thin spoon-shaped toenails. This mostly affects his great toenails, but his other toenails are also affected. His fingernails are normal.
 |
Spoon-shaped Nails in 3 Year Old |
His sibling has normal nails. His father says the boy occasionally complains of pain from his toenails. Any workup or treatment options?
.
Scott Werter, DPM, Myrtle Beach, SC
05/23/2009
QUERIES (CLINICAL)
Query: Charcot Foot and Gout
I recently had a mid-60's female diabetic present with what appeared to be late stage Charcot foot deformities with the typical midfoot destruction of navicular and cuneiforms, LisFranc's type lateral dislocation of the lesser metatarsals, and rocker bottom appearance. She also noted that she had been treated for chronic systemic gout for the past year and a half. She underwent a CT scan and the radiologist noted that the midfoot destructive changes appeared consistent with an inflammatory arthritis such as gout.
Prior to this, I've had two or three other patients over the past year that had what appeared to be Charcot changes of the foot along with severe tophaceous gouty arthritis. I do not recall any particular connection between the two, so is this a frequent occurrence, and is it possible for chronic gout to cause the same pattern of bone destruction and collapse of the foot like Charcot? If so, would the resulting foot deformities be treated like Charcot feet?
Leonard Kuzmicki, DPM, Spring Valley, IL
05/20/2009
QUERIES (CLINICAL)
RE: EMLA Toxicity
From: Philip Wrotslavsky, DPM
With regard to the discussion of topical anesthetics such as EMLA, I am reminded of what Dr. John Herzenberg used to teach us before doing tenotomies on Ponseti-cast clubfeet. EMLA has a toxic dose and we need to be aware of that. EMLA- lidocaine2.5% + prilocaine 2.5% toxicity of lidocaine –methemoglobinemia MHG precipitated by Tylenol, phenytoin, toxic dose (< 3months) = 1gram/10cm2/hour Typical tube = 5 grams RX for methemoglobinemia = methylene blue.
There are reported cases of EMLA toxicity.Here is one (just Google "EMLA toxicity" for the rest) 2004: Parker James F; Vats Atul; Bauer Greg EMLA toxicity after application for allergy skin testing. Pediatrics 2004;113(2):410-1. Lidocane toxicity may be observed at 6 mcg/mL 1 cc of 1% Lidocaine = 10 mg 4 kg baby… 12-20 mg… 1-2 cc only! The bottom line is whether you believe children have pain or remember pain, know well what you are giving them.
Philip Wrotslavsky, DPM, La Jolla, CA, drphilipw@msn.com
05/19/2009
QUERIES (CLINICAL)
Query: Reverse Weil Osteotomy
I have a patient with no fourth met head and severe pain at the 3rd and 2nd met head regions. She is too young for a Hoffman procedure and she has not responded to off-loading of the site. Does anyone have any experience with a reverse Weil osteotomy; instead of cutting the metatarsal from distal dorsal to proximal and plantar, cutting the metatarsal proximal to the neck and aiming plantar and distal to slide the head proximally and dorsally?
Robert S. Mandresh, DPM, Indianapolis, IN
05/18/2009
QUERIES (CLINICAL)
Query: Posterior Tibial Tenosynovitis
I treated a 58 y/o lady with HTN, for posterior tibial tenosynovitis successfully with immobilization and Voltaren; and followed up with functional orthotics for her abnormal pronation. She has had the orthotics since 2/09 and was doing well in March. She returned in early May compaining of severe pain in her feet in spite of wearing the orthotics. She says the pain is different and in different areas; not always the same. She further describes pain as “burning shock sensation.” Her MD ran RA, Vit D, Lyme and thyroid tests; all normal/negative. She has more pain with more activity and it is worse without the supports. She denies any rashes or other spontaneous bodywide muscle-skeletal pain.
I found no pedal inflammatory signs on recent exam and no pain triggers, including in the PT tendons, plantar fascia, or lateral sinus tarsi. I would like thoughts on further work-up. I am considering ordering a bone scan to confirm local inflammatory process vs. non-pedal/neuro cause for the symptoms.
Mark Aldrich, DPM, Antigo, WI
05/16/2009
QUERIES (CLINICAL)
Query: Disease of Toenails in 3 Year Old
The mother of this 3 year old female is currently debriding her nails at home with a Dremel tool. I have recommended that if nothing else can be found to work, then I would recommend removal of the medial and lateral borders. I drew this area out using a small black felt marker to show her that we would be removing just the borders.
 |
Disease of Toenails in 3 Year Old |
The patient has tried urea cream. Carmol gel 4 was Rx’d but local pharmacies are unable to get this. Her father has similar nails. Is there anything else that should be done?
H. Ashley Ledger, DPM, Killeen, TX, drledger@hot.rr.com
05/15/2009
QUERIES (CLINICAL)
Query: Osteotomy?
We have a female patient in her 40s with an IM angle 12-13 degrees (factoring in her metatarsus adductus). The met protrusion is zero, so the 1st and 2nd metatarsals are equal in length. There is also a 2nd digit symptomatic hammertoe deformity and there is sub-met 2 pain with callus formation.

|
Osteotomy? |
When would one decide to do a 2nd metatarsal osteotomy? If so, which procedure specifically?
Margaret Portela, DPM, Union City, NJ
05/14/2009
QUERIES (CLINICAL)
Query: Spider Bite Complications
I have a 44 y old patient who was bitten (or so he thinks) by a brown recluse spider about seven years ago. Once the wound was resolved (sx excision), the wound showed up on the other leg. The patient states the new wound had the same presentation as the original wound and he is sure he was not bitten again. Now he says every Spring the wound returns, most often at the original site. I am aware that most spider bites are in actuality infections and most commonly Staph infections, but I am just curious if anyone else has seen or heard of spider bite wounds returning or going to the other leg/foot?
.jpg)
|
Spider Bite Complication |
The patient has venous stasis, but the wound is atypical for venous stasis, and it is not in the normal location (wound is anterior lateral calf, about mid shaft). The presenting erythema is not centered around the wound, but is usually more around the lower posterior calf, well above the ankle. The local temperature of the calf was 103.1. Ultrasound was negative for DVT, less than 1+ pitting edema. DP/ PT WNL. Systemic fever 101. Significant for varicose veins and chronic edema, but he wears support hose. No other health factors. He responded well to doxycycline. Work up for PG was negative.
Wm. Barry Turner, DPM, Royston, GA
05/13/2009
QUERIES (CLINICAL)
Query: Diabetic Ulcer Sub-met 3
This is a fragile diabetic patient that has had multiple surgeries on her right 3rd metatarsal. The head was ultimately removed and she did well for several years. She now has a crevice in her foot sub-met 3, and is starting to break down sub-met 4 as well.
.jpg) |
Ulcer Sub Met 3 |
Any thoughts on how to proceed with this patient would be appreciated. She cannot afford to be out of work for an extended period of time.
.jpg) |
Ulcer Sub-Met 3 |
Rick Burnell, DPM, Camden, SC
05/12/2009
QUERIES (CLINICAL)
Query: TOG Gait Scan
Does anyone have experience with the TOG Gait Scan?

|
TOG Gait Scan |
Rich Resnick, DPM, Burke, VA