





|

|
|
|

|
Search
04/24/2013
HEALTHCARE NEWS
AMA Initiative to Target Diabetes, Heart Disease
By working with ongoing national campaigns and “galvanizing America's physicians,” the American Medical Association will be seeking to reduce the deaths and healthcare costs associated with cardiovascular disease and type 2 diabetes. Dr. Jeremy Lazarus, president of the AMA, said the organization has earmarked $6 million for the first year of its multi-year Improving Health Outcomes initiative, which could continue for a decade or more.
The AMA will also partner with YMCA of the USA and the Centers for Disease Control and Prevention to target adults whose blood sugar is higher than normal but not yet diabetic. The AMA will support the CDC's National Diabetes Prevention Program. It will also work with physicians to direct their pre-diabetes patients to YMCA diabetes-prevention programs.
Source: Andis Robeznieks, Modern Healthcare [4/22/13]
Other messages in this thread:
07/15/2025
HEALTHCARE NEWS
Distinction Between MDs and Dos Has Become Less Relevant: NY Times
A New York Times article explores the growing presence and evolving role of Doctors of Osteopathic Medicine (DOs) in the U.S. healthcare system. The number of DOs has risen sharply, driven by increasing demand for healthcare providers and limited slots at traditional medical schools. Osteopathic schools have expanded, especially in underserved and rural areas, and now train more than a quarter of all U.S. medical students. DOs tend to focus more on primary care, and their education emphasizes a holistic approach and manipulative treatment techniques, though fewer than half still use those hands-on methods today.
Despite some differences in training emphasis and admissions criteria, DOs and MDs now largely share the same responsibilities, from prescribing medication to performing surgery. Their education overlaps significantly, and many DOs attend the same residencies and take the same board exams as MDs. While DOs may face more challenges entering highly competitive specialties, studies show comparable patient outcomes between the two professions. The author concludes that the DO vs. MD distinction has become less relevant and suggests that qualities like availability and communication matter more when choosing a physician.
Source: Teddy Rosenbluth, The New York Times [7/13/25]
05/16/2025
HEALTHCARE NEWS
Cleveland Clinic’s Controversial New Policy: Pay Co-pays Upfront or Lose Your App't.
Starting in June, Cleveland Clinic patients who can’t pay their co-pay on the spot will have non-emergency appointments rescheduled or cancelled, the health system said.
The new policy could make it harder for low-income people who prefer to be billed to see a clinic doctor, and create delays that could lead to medical emergencies down the road, health policy experts said. A delay in care can mean six to eight more weeks of a tumor growing or a blood clot developing.
Source: Julie Washington, cleveland.com [5/13/25] via Dr. Seymoure Balaj
05/28/2024
HEALTHCARE NEWS
WHO Updates List of Most Dangerous Drug-Resistant Pathogens
For the first time in seven years, the World Health Organization has updated its list of the most dangerous, antimicrobial resistant pathogens. The revised list includes 24 pathogens from 15 different families of antibiotic-resistant bacteria. The revision was prompted by the growth of the problem. There were approximately 4.95 million deaths caused by antibiotic resistance across low- and middle-income countries in 2019 alone, according to the May 17 report.
New this year, is the inclusion of Gram-negative bacteria that are resistant to last-resort antibiotics, which the WHO calls special attention to. In its 2024 update, the WHO removed five pathogens that were listed in 2017, including: penicillin non-susceptible Streptococcus pneumoniae, vancomycin-resistant Staphylococcus aureus, fluoroquinolone-resistant Campylobacter, clarithromycin-resistant Helicobacter pylori, and third-generation cephalosporin-resistant Providencia. There were three new additions to the list: macrolide-resistant Group A Streptococci, penicillin-resistant Group B Streptococci, and rifampicin-resistant Mycobacterium tuberculosis.
Source: Ashleigh Hollowell, Becker's Hospital Review [5/24/24] via Dr. Allen Jacobs
05/23/2024
HEALTHCARE NEWS
A New Emerging Fungal Threat
Researchers in New York have found an emerging threat of ringworm fungus, Trichophyton indotineae, which is often resistant to standard therapy, according to a study published May 15 in JAMA Dermatology. The fungus has been detected worldwide, but data is sparse for its spread in the U.S., the researchers said. In May 2023, public health officials reported the first two confirmed T. indotineae cases in the U.S., but antifungal susceptibility testing data uncovered more infections, spanning back to 2017.
From May 2022 to May 2023, 11 patients in New York City had confirmed T. indotineae infections, and nine reported previous travel to Bangladesh. All had widespread lesions, diagnostic delays, and did not respond to antifungal monotherapies. Terbinafine, the preferred treatment, was ineffective for seven patients. Patients treated with fluconazole and griseofulvin improved in two of four and two of five instances, respectively, and itraconazole was effective for five of seven treated patients. Since these cases happened before May 2023, dermatologists were often unaware of T. indotineae at the time of treatment, the researchers said.
Source: Paige Twenter, Becker's Hospital Review [5/20/24] via Dr. Allen Jacobs
05/20/2024
HEALTHCARE NEWS
Weight Loss Drugs Could Bankrupt Healthcare System: Sanders
Weight loss drugs have the potential to bankrupt the U.S. healthcare system, according to a May 15 report from Sen. Bernie Sanders' office. Mr. Sanders chairs the Senate Committee on Health, Education, Labor, and Pensions, which opened an investigation into Novo Nordisk's list prices for Ozempic and Wegovy in April. Medicare total spending hit $5.7 billion in 2022 for GLP-1s, up from $57 million in 2018, according to a March analysis from KFF.
"Today's report makes it crystal clear: The outrageously high price of Wegovy and other weight loss drugs have the potential to bankrupt Medicare and our entire healthcare system," Mr. Sanders said. "The unjustifiably high prices of these weight loss drugs could also cause a massive spike in prescription drug spending that could lead to an historic increase in premiums for Medicare and everyone who has health insurance." Novo Nordisk charges $969 per month for Ozempic in the U.S., compared to $155 in Canada, $122 in Italy, $71 in France and $59 in Germany. The Danish drug manufacturer lists Wegovy for $1,349 per month in the U.S.
Source: Jakob Emerson, Becker's Hospital Review [5/26/24] via Dr. Allen Jacobs
05/17/2024
HEALTHCARE NEWS
The 10 Top Causes of Death for Adults in the U.S.
1. Heart disease 267.2*
2. Cancer 142.3
3. Unintentional injuries 64.0
4. COVID-19 44.5
5. Stroke 39.5
6. Chronic lower respiratory disease 34.3
7. Alzheimer disease 28.9
8. Diabetes 24.1
9 Kidney disease 13.8
10. Chronic liver disease and cirrhosis 13.8
*Deaths per 100,000 population
S8ource: Jeffrey Bendix, Medical Economics [5/15/24]
05/15/2024
HEALTHCARE NEWS
Hospitals Are Refusing to Do Surgeries Unless You Pay in Full First
For years, hospitals and surgery centers waited to perform procedures before sending bills to patients. That often left them chasing after patients for payment, repeatedly sending invoices and enlisting debt collectors. Now, more hospitals and surgery centers are demanding patients pay in advance. Advance billing helps the facilities avoid hounding patients to settle up. Yet it is distressing patients who must come up with thousands of dollars while struggling with serious conditions.
Those who can’t come up with the sums have been forced to put off procedures. Some who paid up discovered later they were overcharged, then had to fight for refunds. Among the procedures that hospitals and surgery centers are seeking pre-payments for are knee replacements, CT scans, and births.
Source: Melanie Evans, The Wall Street Journal [5/10/24]
05/13/2024
RESPONSES/COMMENTS (HEALTHCARE NEWS)
RE: Two Huge Healthcare Stories
From Paul Kesselman DPM)
In yesterday’s Becker's Health Care Newsletter, it is reported that a large multi-state hospital system is suing Multiplan for illegal price fixing and automatic significant price reductions, in particular, for out-of-network providers. The story states that Multiplan, by bombarding healthcare providers with automatic reductions in pricing, has made it impossible for providers to deliver healthcare.
The second story impacting healthcare providers has to do with Change Health Care, one of the largest healthcare providers in the country. NYC Health and Hospitals is moving away from Change Health Care. Other stories earlier this week had the CEO of Optum (which owns Change) on the hot seat at a Congressional Hearing. One of the charges made against Change, was that they ignored previous warnings and failed to implement simple systems such as MFA.
Paul Kesselman, DPM, Oceanside, NY
04/29/2024
HEALTHCARE NEWS
Oregon Physician Assistants Get Name Change
On April 4, Oregon’s Governor Tina Kotek signed a bill into law that officially changed the title of “physician assistants” to “physician associates” in the state. The switch is the first of its kind in the United States and comes on the heels of a decision from 2021 by the American Academy of Physician Associates (AAPA) to change the meaning of “PA” to “physician associate” from “physician assistant.”
In the Medscape Physician Assistant Career Satisfaction Report 2023, a diverse range of opinions on the title switch was reflected. Only 40% of PAs favored the name change at the time, 45% neither opposed nor favored it, and 15% opposed the name change, reflecting the complexity of the issue. According to the AAPA, the change came about to better reflect the work PAs do in not just “assisting” physicians but in working independently with patients.
Source: Jennifer Nelson, MDedge [4/26/24]
04/22/2024
HEALTHCARE NEWS
Feds Open Online Portal for Reporting Anticompetitive Practices in Healthcare
Federal agencies want to hear from the public about monopolistic and anticompetitive behavior within the healthcare industry. Thursday, the Federal Trade Commission (FTC), the Department of Justice (DOJ) and the Department of Health and Human Services (HHS) unveiled HealthyCompetition.gov, an online portal where anyone can submit a healthcare competition complaint for potential investigation.
These submissions, the agencies said, can help the agencies ensure healthcare organizations provide quality care and pay their employees a fair wage.
Source: Dave Muoio, Fierce Healthcare [4/18/24]
04/19/2024
HEALTHCARE NEWS
Lawmakers Express Fury Toward UnitedHealth in Change Attack Hearing
UnitedHealth Group drew the ire of federal lawmakers during the first hearing on the fallout surrounding the unprecedented cyberattack on Change Healthcare in late February. Individuals representing the American Hospital Association, private cybersecurity groups and providers testified before members of the House Energy and Commerce Committee on April 16 to discuss the healthcare industry's response to the attack and how the federal government should act.
In March, the cybercriminal organization received $22 million in bitcoins, though UnitedHealth Group has not addressed whether the company paid the ransom. On April 15, ransomware group RansomHub posted files on its dark web leak site comprising of personal and protected health information on patients whose data was taken in the hack. The files also include contracts and agreements between Change and its clients, marking the first time hackers have posted data from the attack.
Source: Jakob Emerson, Becker's Hospital Review [4/17/24] via Dr. Allen Jacobs
04/10/2024
HEALTHCARE NEWS
MultiPlan: Health Insurers’ Lucrative, Little-Known Alliance
Large health insurers are working with a little-known data company to boost their profits, often at the expense of patients and doctors, a New York Times investigation found. A private-equity-backed firm called MultiPlan has helped drive down payments to medical providers and drive up patients’ bills, while earning billions of dollars in fees for itself and insurers.
The most common way Americans get health coverage is through an employer that pays for workers’ medical care itself and uses an insurance company to administer the plan. Providers in the plan’s network have agreed-upon rates, but out-of-network providers often must negotiate payments. By using MultiPlan’s frugal recommendations, insurers say they are saving employers money. But insurers and MultiPlan also benefit because their fees are typically based on the size of the declared “savings” or “discount” — the difference between the original bill and the amount actually paid. In some instances, insurers and MultiPlan have collected more for processing a claim than the provider received for treating the patient.
Source: Chris Hamby, The New York Times via Dr. Fred Ferlic
04/05/2024
HEALTHCARE NEWS
Physicians Received $12 Billion from Drug & Device Makers in Less Than 10 Years
A review of the federal Open Payments database found that the pharmaceutical and medical device industry paid physicians $12.1 billion over nearly a decade. Almost two thirds of eligible physicians — 826,313 doctors — received a payment from a drug or device maker from 2013 to 2022, according to a study published online in JAMA on March 28. Overall, the median payment was $48 per physician.
Source: Alicia Ault, MD Edge [4/3/24]
11/21/2023
HEALTHCARE NEWS
Ozempic Sparks Controversy on Surgery Prep
With the increase of prescriptions for glucagon-like peptide-1 receptor agonists like Ozempic, Mounjaro, and Wegovy, physicians began seeing a startling number of regurgitation and aspiration in surgeries. GLP-1s delay gastric emptying, meaning normal fasting rules weren't cutting it. In response to anecdotal reports and case studies, the American Society of Anesthesiologists published a guideline in June recommending patients stop taking GLP-1s within the half life period — such as skipping one week's semaglutide injection — before undergoing anesthesia.
There's one area resulting in a "clinical dilemma," according to the AGA. Christopher C. Thompson, MD, who helped draft the gastroenterological group's Nov. 7 statement, said after the ASA's June guidance, "many of our cases were being canceled, and this was problematic for patients."
Source: Paige Twenter, Becker's Hospital Review [11/16/23] via Dr. Allen Jacobs
07/21/2023
HEALTHCARE NEWS
Docs Urge Congress to Step in as CMS Proposes Cuts to Payments
The Biden administration is proposing cuts to physician payments in its annual fee schedule, and doctors are not happy. Major industry groups have roundly called for Congress to step in to prevent the Medicare reimbursement changes from going through. Last week, the Centers for Medicare & Medicaid Services (CMS) proposed a 3.34% cut to the fee schedule's conversion factor, which is used to calculate Medicare payouts to docs.
In a statement, the American Medical Group Association (AMGA) said that Medicare payments already fail to keep up with "the increasing cost of delivering healthcare," and further cuts would only exacerbate that problem. “AMGA members cannot absorb this proposed payment cut,” said AMGA President and CEO Jerry Penso, MD. “Their expenses are continuing to increase, and Congress needs to act to ensure Medicare’s reimbursement reflects the cost of delivering high-quality care to patients."
Source: Paige Minemyer, Fierce Healthcare [7/17/23]
05/15/2023
RESPONSES/COMMENTS (HEALTHCARE NEWS)
From: Bret Ribotsky, DPM
It’s important to note that Trichophyton indotineae is resistant to oral terbinafine and should be treated with oral itraconazole. Itraconazole must be taken with meals and has many side-effects, including possible heart failure. It should not be taken with alcohol.
Bret Ribotsky, DPM, Fort Lauderdale, FL
05/13/2023
HEALTHCARE NEWS
First Reported U.S. Cases of Tinea Caused by Trichophyton Indotineae
Two cases of highly contagious, drug-resistant ringworm infections have been detected in New York City – the first such cases reported in the United States, the Centers for Disease Control and Prevention reported Thursday. This “infection was first identified in a 47-year-old woman who had developed a bad case of ringworm, also known as tinea, while traveling in Bangladesh,” after “a rash had erupted across most of her body and typical antifungal creams did nothing to alleviate it.” Her “infection turned out to be caused by a relatively new species of ringworm-causing fungus, called Trichophyton indotineae.
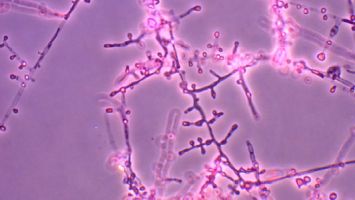 |
Trichophyton indotineae |
Another woman, “had no recent international travel history,” and “neither of the women had underlying health conditions.” The discovery of these “infections is worrying for public health officials as they are the first reported in the U.S., after cases had been reported in Asia, Europe, and Canada.” In particular, “the CDC said the fact that the woman who had no recent international travel history was found to have the infection was alarming, indicating it could be a ‘potential local U.S. transmission.’” As such, “the agency said healthcare providers should be prepared to provide up to 12 weeks of therapy if the fungus that causes the condition is found.
Sourec: CDC via NBC News, The Hill via Drs. John Evans and Robert Creighton
03/23/2023
HEALTHCARE NEWS
Candida Auris Spreading At “Alarming Rate” In Health Facilities, CDC Says
The Washington Post reports “a deadly and highly-drug resistant fungus is spreading at ‘an alarming rate’ in long-term care hospitals and other health facilities caring for very sick people, the Centers for Disease Control and Prevention announced Monday.” Fungal infections tied to “the yeast strain known as Candida auris tripled nationally from 476 in 2019 to 1,471 in 2021, according to CDC data.”
In the same time period, “cases where a person carries the fungus but is not infected nearly quadrupled from 1,077 to 4,040.” Preliminary data suggest “the numbers have continued to rise.” The findings were published in the Annals of Internal Medicine.
Source: Fenit Nirappil, Washington Post [3/20/23] via The Daily
03/22/2023
HEALTHCARE NEWS
"Black Boxes" Make Their Way into Hospital ORs
Twenty-four hospitals in the U.S., Canada, and Western Europe are using "black boxes" — named after the recording devices in airplanes — to collect and analyze operating-room practice data in hopes of reducing medical errors and improving patient safety and operating room efficiency, The Wall Street Journal reported March 19.
The OR Black Box, made by Surgical Safety Technologies in Toronto, gathers video, audio, patient vital signs and data from surgical devices during surgery. Audio and video are de-identified, giving participants blurred faces and cartoonish bodies, according to the report. Hospitals can use the data to view performance over time or to analyze particular operations.
Source: Mariah Taylor, Beckers Hospital Review [3/20/23] via Dr. Allen Jacobs
10/19/2022
HEALTHCARE NEWS
25% of Clinicians Want Out of Healthcare: Survey
One quarter of U.S. physicians, advanced practice providers, and nurses are considering switching careers and one third are considering switching employers, according to newly released results from a survey conducted by Bain & Company. Below are some key takeaways from the survey and brief, which was released Oct. 11 and can be found in full here.
1. Of the 25 percent of clinicians who are thinking about exiting healthcare entirely, 89 percent cite burnout as the main driver.
2. The top three things clinicians care about most in their profession are compensation, quality of patient care, and workload, according to the survey. Of those three, they are least satisfied with compensation (59 percent expressed satisfaction) and workload (60 percent). Eighty percent said they are satisfied with the quality of patient care.
3. Burnout shows up throughout clinicians' days, with 63 percent saying they feel worn out at the end of the workday, 51 percent saying they feel they don't have time and energy for family and friends during leisure time, and 38 percent feeling exhausted in the morning at the thought of another workday.
Source: Molly Gamble, Becker's Hospital Review [10/11/22] via Dr. Allen Jacobs
01/28/2022
HEALTHCARE NEWS
ONC Looks For Comments on How to Improve Prior Authorization
The Office of the National Coordinator (ONC) for Health Information Technology is taking aim at one of the prime pain points for clinicians, providers, payers, and patients – the prior authorization process. Finding standards and using them, which would enable organizations to use data exchange to automate at least some of the prior authorization process would help improve patient safety, ensure continuity of care, reduce administrative burden, and help relieve clinician burden.
ONC last week announced that it is seeking public comment on electronic prior authorization standards, implementation specifications, and certification criteria that could be adopted within the ONC Health IT Certification Program. “Responses to this (Request for Information) may be used to inform potential future rulemaking to better enable providers to interact with healthcare plans and other payers for the automated, electronic completion of prior authorization tasks,” the ONC announced.
Source: HealthData Management [1/26/22]
09/18/2021
HEALTHCARE NEWS
Docs Press CMS for Permanent Telehealth Flexibility, Relief from Pay Cuts
Several doctor groups are pressing the Biden administration to not just extend Medicare telehealth reimbursement flexibilities through 2023 but for them to be made permanent. The Centers for Medicare & Medicaid Services proposed in the 2022 Physician Fee Schedule to extend telehealth flexibilities through 2023 instead of through the end of the COVID-19 public health emergency, which is expected to run through this year. Doctor groups in comments on the rule, the deadline for which expired Monday, called for a permanent solution.
Doctor groups were also worried about a looming 3.75% cut in the 2022 Medicare conversion factor, which calculates reimbursement for procedures under fee-for-service. The cuts are mandated under a budget neutrality provision in Congress and comes after a pay bump from Congress that expires in 2022. MGMA said that the cuts are going to be especially difficult on physician practices as other cuts could come into effect, such as a 4% payment cut to Medicare reimbursements under the PAYGO law that mandates cuts if federal spending reaches a certain level. Physicians also must likely brace for the return of a 2% cut to payments that was installed under the sequester. The cut has been put on pause for more than a year due to the pandemic, but lawmakers seek to use it as a pay-for in a bipartisan infrastructure bill expected to be considered in the House later this month.
Source: Robert King, Fierce Healthcare [9/14/21]
07/14/2021
HEALTHCARE NEWS
New NSF Center Aims to Shift to Home-Based Healthcare
Caltech, the University of Arizona, Baylor College of Medicine, and USC have joined together to create a new National Science Foundation (NSF) center that aims to shift healthcare from a model that requires patients to receive care in a hospital or doctor's office to a model in which patients manage their health from home. The team is moving forward with a commitment to remote care that is stronger than ever.
 |
Dr. David Armstrong |
"The proposal brings together quite a lot of potential research and industry firepower to focus on an area that couldn't be more primed for innovation," said Dr. David G. Armstrong, director of the USC site and professor of surgery and director of the Southwestern Academic Limb Salvage Alliance. "We really have the potential to develop some of the basic foundations about how we merge consumer electronics and medical devices moving forward. Working with early-stage startups all the way up to the biggest of the big tech is such a spectacular gift. We look forward to paying it forward."
Source: Caltech [7/8/21]
07/08/2021
HEALTHCARE NEWS
Devicemakers Have Funneled Billions to Orthopedic Surgeons
Health policy experts and regulators have focused for decades on pharmaceutical companies’ payments to doctors — which research has shown can influence which drugs they prescribe. But far less is known about the impact of similar payments from device companies to surgeons. A drug can readily be stopped if deemed harmful, while surgical devices are permanently implanted in the body and often replace native bone that has been removed.
Every year, a torrent of cash and other compensation flows to these surgeons from manufacturers of hardware for spinal implants, artificial knees, and hip joints — totaling more than $3.1 billion from August 2013 through the end of 2019, a Kaiser Health News analysis of government data found. These bone specialists make up a quarter of U.S. doctors who have accepted at least $100,000 or more, and two-thirds of those who raked in $1 million or more from the medical device and drug industries last year, the data shows.
Source: Fred Schulte and Elizabeth Lucas, Kaiser Health News via Dr. Allen Jacobs
06/04/2021
RESPONSES/COMMENTS (HEALTHCARE NEWS)
From: Elliot Udell, DPM
If a person has PVD in their lower extremity and he or she is not on a statin drug, should we be putting them on a statin to prevent further deterioration? To date, I have been sending them back to primary care, but should podiatry be looking at prescribing statins for patients with PVD affecting the feet?
Elliot Udell, DPM, Hicksville, NY
|
| |

|
|
|







